In the 1990s, there was a small, quiet revolution in American health care that promised to be as far reaching as the advent of antidepressants like Prozac. The revolution involved a new class of medications called atypical antipsychotics, designed for the treatment of schizophrenia.
The atypicals were an instant hit with doctors and schizophrenics alike. Initially, the drugs treated schizophrenia far better than older drugs like Thorazine and Haldol had done. In mental-health circles, atypicals were sometimes referred to as “the silver bullet,” the breakthrough to a centuries-long quest to effectively treat the most vicious of mental illnesses without turning patients into zombies.
But now this is a revolution in trouble.
The new meds don’t work as well for schizophrenics as their initial rock-star status suggested, according to recent research. Questions about their effectiveness are now being raised. At the same time, these very same meds are being handed out like candy to a different class of patients: the millions of Americans with bipolar disorder, or good old manic-depression. We are not talking about people in psych hospitals or on the brink of suicide. We are talking about people with plain vanilla bipolar disorder—the kind where you can’t sleep and are wound up for days but are a long way from diving off a bridge or running naked down the street.
In other words, fairly regular, mainstream Americans now take the most powerful mood-altering drugs in all of psychiatry. Last year, 23 million prescriptions were written for these drugs. Sales this year are expected to hit $10 billion, three times what they were in 2000. Atypicals are the fourth largest class of patented medications in America.
Patients aren’t taking them for a few days or weeks, either. Doctors expect their bipolar patients to take these drugs for years, much the same as they’ve taken traditional mood stabilizers, like lithium, which tamp down mood swings. In fact, there’s a growing rumble in the psych world that researchers would like to use atypicals to replace mood stabilizers altogether.
Yet there is no comprehensive scientific evidence to support this paradigm shift. Zero. The psychiatric industry says this isn’t a problem because real-world treatment has always outpaced research. But if you happen to be a patient, it’s a very big problem—atypicals have the worst side effects of any drugs used to treat bipolar disorder. As a patient, I’ve experienced this shift firsthand, sometimes as a willing test subject. So, I have a question: Without scientific evidence, why are doctors prescribing these meds so freely and expecting patients to take them for so long?
For the past 15 years, psych meds have been touted as the answer for every flaw of mood, feeling, and behavior in American society. We are in the midst of what’s called the psychopharmacological revolution, a shift from the days of nasty meds that didn’t work well to new generations of meds that aren’t nasty and work very well. That’s the hype, at any rate. But the revolution isn’t playing out as advertised.
Even the habitually cautious National Institute of Mental Health (NIMH) now says that psych meds—including atypicals—only work 50 percent of the time.
But the mental-health world is congenitally incapable of being skeptical about how psych meds work in patients’ lives. Doctors quickly become wedded to new therapies, and patients follow. As a result, a new treatment paradigm for millions of bipolars is charging ahead when researchers, doctors, and patients ought to be very cautious.

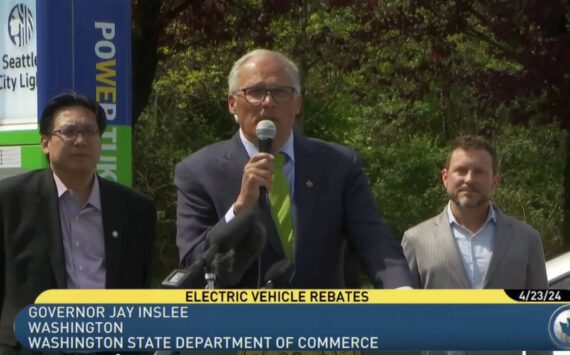
A new class of drugs for treating mental illness, atypical antipsychotics are becoming more widely used. Sales this year are expected to hit $10 billion.
(Jay Vidheecharoen) |
Bipolar patients should be asking why doctors want them to use meds long term that regularly generate debilitating side effects in both bipolars and schizophrenics—the kind of side effects that can mess with a patient’s life almost as much as the underlying illness. Last summer, Eli Lilly quietly and with little media notice settled a lawsuit for $750 million. The suit alleged that patients had injuries, including diabetes, caused by Zyprexa, the top-selling atypical in the world. Reportedly, 23 patients have died as a result of using the drug.
All psych meds generate side effects, but atypicals even more so. On these meds, patients can gain 20 to 40 pounds in a year. Blood sugar levels shoot upward. Cholesterol goes up as well. The question of side effects is important not only because of short-term comfort, but because of patients’ long-term physical health. Extreme weight gain and altered blood cholesterol levels, for example, give rise to what doctors call the “metabolic syndrome,” a fancy way of saying underlying cardiac and respiratory problems can be caused by these medications over time.
That’s not speculation, either. Recently published long-term data on schizophrenics taking atypicals showed weight gain on the order of 2 pounds a month, for example. Researchers say the same dynamic is present in bipolars. Any patient who takes atypicals can tell you all about those effects. To date, however, there have been no long-term studies of the effects of these medications on bipolar patients. There are other effects, too, life-reducing ones. The daylong grogginess that comes with atypicals like Seroquel. Cognitive slowing. Risperdal’s tendency to stiffen faces. An odd sense that somehow you aren’t the same person you were before. There’s something about the immediacy of sensation that changes. Nothing is as vivid as it was before. You feel calm and diluted at the same time.
The goal of mental-health treatment is to enhance human life, not limit it.
But something else about long-term treatment of bipolar disorder with atypicals is as troubling as the side effects. These powerful meds don’t do a good job of knocking down symptoms over the long term. In the five years that atypicals have been used aggressively in treating the disorder, I have only encountered a handful of patients who say that their original starter dose of Zyprexa, say, wiped out their mania and depression and that life has been balanced ever since.
More commonly, patients will start on an atypical after failing to see their symptoms disappear, or remit, on more traditional meds—and that happens all the time. The atypical will perform well for a few months, but then for many bipolars, the symptoms roar back to life. They begin cycling out to the manic fringes again. Their minds race, they cannot sleep, they fall apart. That’s the nature of the bipolar beast— limited symptom remission.
Let’s talk best-case scenario: They are self-aware, responsible patients and recognize what is happening. They go see their doctor. As often as not, that’s a general practitioner or internist instead of a psychiatrist. The doctor’s common response will be to either increase the dosage or switch the patient to another atypical. Within a few months, the process will be repeated because the patient has had yet another bout of hypomania, a restless state of insomnia and racing thoughts.
I know bipolars with fairly moderate forms of the illness who have been on three different atypicals in three years. (There are five commonly used atypicals; see chart, this page.) They have gone through multiple dosages of each—and they are usually taking a mood stabilizer and an antidepressant at the same time.
I am not the only bipolar who finds this medication and dosage switching to be unacceptable.
Mental-health experts typically wave away such complaints by saying, “Each patient is an individual and responds differently to different medications, and patients must often switch from medication to medication to find the treatment that works best for them. There are medications that will work well for you. There is hope.”
Doctors, researchers, and advocates have trotted out the same line since the psychopharmacological revolution hit the American mainstream about 15 years ago. Its implied promise was that taking new-generation psych meds would remit symptoms forever. Applied to mood stabilizers and antidepressants, which have comparatively lesser side effects, the promise doesn’t sound like much more than harmless cheerleading. But when the same logic is applied to atypicals, it sounds irresponsible and coldhearted because, with their rotten side effects, they still fall short of the goal. The name alone tells you that atypicals are a wholly different class of drugs. All of these meds carry FDA-required black-box warnings because their use can cause diabetes.
Atypical antipsychotics are major juju—a kick in the brain, the purple pill that puts you on the floor, the white pill that turns your face stony. Some patients pine for the side effects of lithium and Lexapro, which are benign by comparison.
I say none of this lightly.
I’ve lived with bipolar disorder for 16-plus years. I have taken all the major medications at one time or another. In that time, I have interviewed, talked with, counseled, and basically hung out with hundreds of bipolars, schizophrenics, and depressives. Few of us have ever seen the promise of the psychopharmacological revolution fully realized, except for short bursts at a time.
Much of what has become standard long-term treatment, or maintenance, in mental illness is based on short-term studies. The FDA doesn’t require long-term tests in order to license medications. As a result, most psych meds are typically studied in eight- to 12-week trials. That tells doctors about patients’ short-term response and little more. There is little incentive for drug companies to fund further studies. The federal government rarely steps into the breach to fund long-term studies, either.
But most psychiatry involves giving patients drugs for maintenance, not to bail them out of a short-term crisis. Absent long-term data, maintenance becomes more of an art than science, though psychiatrists and doctors don’t like to admit that, especially to patients sitting in their office.
There is a disconnect here that makes patients sitting ducks. Their illness is lifelong not short term.
Patients are often downright desperate when they see their doctor, especially if they’ve had a recent relapse—one of the most annoying aspects of the disorder is that symptoms will re-emerge at some point, even if you strictly adhere to treatment.
Besides trying to find a treatment that works, patients are also trying to placate competing interests. Families and friends press them to find some kind of medication that works—take anything! Employers warn they are on thin ice. If they don’t find something that works, then they are likely to be bounced right out of American life.
They’ll take damn near anything a psychiatrist or general practitioner suggests to get a short-term result. That’s potentially millions of patients going to their doctors each year looking for something— anything—that works. Often, these same patients find that the next something doesn’t work, either.
Nice psychopharmacological revolution we’ve got.
The irony is that as problematic as atypicals are for bipolars, they are the best deal schizophrenics have ever seen. Until the 1950s, schizophrenics were treated in some of the most inhumane ways imaginable. Tied to a bed for weeks on end. Padded rooms. Lobotomies. None of that worked very well.
Then along came Thorazine, Haldol, and a host of other antipsychotics that, in many cases, stopped patients’ hallucinations, paranoia, delusions, and violent outbursts. The trouble was that antipsychotics typically took a huge toll, inducing disabling side effects such as frozen expressions, shuffling gaits, and shaking limbs— zombieism, in effect.
In 1989, a medication called Clozaril hit the world that caused none of these physical side effects. It was dubbed “atypical.” But this medication proved toxic to some patients’ immune systems. As a result, the medication was used sparingly even though it seemed to work better than the older antipsychotics.
By the mid-1990s, newer atypical antipsychotics were introduced. They didn’t have Clozaril’s toxicity. Doctors quickly shifted to the new meds. Within years, atypicals like Zyprexa, Risperdal, and Seroquel almost completely displaced the older drugs. Patients seemed to do well on them—no more tremors, no more frozen stares. Many people were able to get out of state hospitals and restrictive group homes and live fully realized lives in the community.
It was a watershed moment in treating mental illness.
In 2000, sales of atypicals reached $3.2 billion. But already questions had emerged among psychiatrists about just how well these newer meds performed against older antipsychotics, and whether the expense was justified. Atypicals are not cheap—the bill for someone with severe schizophrenia could easily run $1,000 a month, 10 times more costly than the older drugs.
What’s more, doctors and patients documented a new series of side effects from these meds. In particular, patients’ blood sugar levels shot up, cases of diabetes were reported, and patients rapidly gained weight.
The bind for doctors and patients was that there was a complete data vacuum about just how good these meds were or weren’t when it came to maintaining schizophrenia. Doctors also had questions about whether the side effects were as prevalent as many in the business feared.
In 2001, the NIMH funded a $43 million, 1,400-patient study of the long-term performance of four atypicals (Zyprexa, Risperdal, Seroquel, and Geodon) against one old antipsychotic (Trilafon). The CATIE study was the first long-term study of atypicals in schizophrenics. The results were published in the New England Journal of Medicine in September, and generated a fair amount of media attention.
That was because 74 percent of the patients discontinued taking their assigned medication. They either couldn’t handle its side effects or it wasn’t working. This was a startling outcome in light of the decade-long hype around atypicals.
The best of the atypicals in this respect was Zyprexa. Only 64 percent of the Zyprexa patients had to stop taking that drug. Put another way, only 36 percent of the Zyprexa patients found the drug’s performance justified taking it for 18 months. Among the other drugs, Seroquel had the worst discontinuation rate at 82 percent. What’s more, the newer meds didn’t treat schizophrenia’s symptoms much better than Trilafon did, another surprising outcome.
The CATIE study was the shot heard round psychiatry. NIMH went into overdrive trying to explain to the media that the patients didn’t stop taking meds altogether, but switched to something else. Advocacy groups put together media calls and stressed that CATIE wasn’t an indictment of an entire class of meds. Pharma companies issued press releases claiming that their drug was the winner (Eli Lilly’s Zyprexa) and, in one case, that their drug had been used at too low a dosage (Janssen’s Risperdal). The general consensus was that atypicals remain the best treatment available for schizophrenia no matter how side effects cloud their use. No one wants to go back to the bad days of the old antipsychotics.
In the media flurry, no one said a word about bipolars, who now make up 50 percent of the market for atypicals. But there were obvious implications.
As with schizophrenics, the same kind of search for the perfect combination of meds to remit symptoms of bipolar disorder has been going on for decades.
The disorder is marked by extreme mood swings between delusional euphoria and psychosis and the black pit of depression. An estimated 15 percent to 20 percent of bipolars commit suicide. Although the illness was long believed to affect about 3 million Americans, recent estimates double or triple that figure to between 6 million and 9 million.
Bipolar is a tricky illness. It is linked to high levels of intelligence and creativity, for example. Its effects on personality are legendary—uninhibited people-seeking (bipolars are often the life of the party), hypersexuality, and incessant talking, for example.
Classically, the disorder is treated with a mood stabilizer. Lithium was long the gold standard. In recent years, there has been a shift to anticonvulsants like Depakote or Lamictal. Often, bipolars are also given an antidepressant like Paxil or Effexor to deal with bouts of depression. Until 2000, the mood stabilizer plus antidepressant approach was essentially the state-of-the-art treatment. It just doesn’t knock down symptoms forever.
Bipolars can “break through” these meds and wind up having acute episodes of rage or suicidal depression. Another common breakthrough symptom is hypnomania, when the mind races so quickly that the patient cannot sleep for days on end.
In response, doctors loaded patients with higher doses of mood stabilizers and antidepressants. Ten years ago, it wasn’t unusual for a bipolar to end up on 2,500 milligrams of lithium and 60 milligrams of Prozac a day, both fairly high doses. Patients who didn’t respond at those levels would sometimes be given a small dose of an old antipsychotic, if their doctor could trust them. The idea was that patients would use it as needed for a few days until they returned to baseline. Doctors didn’t want patients on antipsychotics for long due to the risk of giving bipolars the same ugly side effects the drugs gave schizophrenics. I was one of those bipolars who was prescribed an antipsychotic, a small dose of Mellaril in my case. I wasn’t even remotely psychotic, in the classic sense of that term. But there was an angry edge that had crept into my daily life (this was in the mid-1990s). On occasion, my mind was too ramped up for me to get anything other than fitful sleep. So, I’d take Mellaril when I was manic or hypomanic and just fog my brain and sleep. That way, I wouldn’t wind up in a hospital, or doing anything that couldn’t be redeemed.
I took 40 milligrams of Mellaril perhaps twice a year. It was never a pleasant experience. Mellaril made me feel leaden and rendered me impotent. Once a girlfriend of mine found the Mellaril in my medicine cabinet. She asked what they were. Nuclear weapons, I told her.
Then I developed paranoia in late 2000. This was a new experience for me, and it dogged me day and night. I knew it had to be addressed quickly before something irreparable happened. So I went to my doctor. He asked me what I knew about antipsychotics, and I told him I was no fan of Mellaril. He suggested the atypical Risperdal. I knew that it was being used by schizophrenics.
“So I take this for a few days?” I figured the deal would be the same as with Mellaril.
“No, you take it all the time,” my doctor answered.
“Why?”
“It doesn’t have the side effects of the old stuff, and you can take it long term to remit your symptoms.”
I’d never heard of antipsychotics being used for maintenance of bipolar disorder. “Are you telling me I’m schizophrenic?”
My doctor told me that his proposal was essentially experimental and off-label. The drug was unstudied in bipolars, nor was it FDA-approved for use in bipolar disorder. But he said there was plenty of anecdotal evidence to support people like me giving it a whirl. And, no, I wasn’t a schizophrenic. So I went to Walgreens and gave it a whirl. Later, I visited the Risperdal Web site. It was devoted to the drug’s use in schizophrenia. I was a guinea pig.
At first, I liked Risperdal. I took it at night along with Depakote and Wellbutrin, an antidepressant. The paranoia disappeared within days. Other than that, the drug kept me calm and made me sleep 10 hours a night. I’d be groggy in the morning. I put on 20 pounds, but I figured it was a small price to pay for ditching that paranoia and buying some peace of mind.
About a year later, my dose went to 1.5 milligrams a day—a baby dose by schizophrenic standards of 4 to 6 milligrams a day—due to a couple of episodes of hypomania that had slipped through the Risperdal curtain. Once again, I had run into the prototypical bipolar complaint of being unable to sleep.
On the higher dose, I felt slowed down and unable to think at my usual clip. This is a common experience for patients taking atypicals long term.
One day, a friend of mine told me that my face had no emotional range. She said I was fixed and stony when I should’ve been smiling. After two years of daily use, the more troubling side effects had blossomed. Weight gain and grogginess I could handle, but not looking emotionless to the world. I had taken psych meds each day for the previous 14 years and was more or less stable, so I decided it was time to be a guinea pig in a whole new way.
In the spring of 2003, I went to my then-doctor and told him I wanted to go off all my meds. I wanted to see what my nonmeds baseline was like.
For three months, things went well. I lost weight, my facial expressions snapped back to life, and my emotions had what seemed like a normal range. Then the edge returned, and I couldn’t sleep. Soon after, I crashed.
My doctor put me back on Depakote and Risperdal. Within a day, I was so agitated I couldn’t sleep and my heart raced. I measured 140 beats a minute at one point. I had to piss every five minutes and was so nauseated that I couldn’t eat. I almost checked myself into Harborview Medical Center for monitoring. I had never had that kind of response to meds of any kind before and I was frightened. When I visited him a couple of days later, my doctor confirmed my hunch that Risperdal was the culprit.
“Let’s replace that with Zyprexa,” he said. I told him no. He gave me samples in case I changed my mind.
Since then, I have continued to chase that edginess and have had occasional bouts of insomnia. My new doctor and I decided last year that I ought to try Seroquel. So I began taking the smallest possible dose.
At first, it helped me sleep, although it took about two hours to be fully alert the next morning. It was as if I had taken a Quaalude and drank a fifth of whiskey the night before. I didn’t like that, neither did I like putting on weight all over again. Seroquel also caused me to have bad dreams—horror-film bad—that I would awake from in full shout. There were mornings where I’d look at myself in the mirror and see scratches on my forehead.
Still, the edge was mostly gone. I liked that. But something about Seroquel bugged me.
Seroquel is very much the med of the moment for treating bipolar disorder. It is made by AstraZeneca. In the last two years, sales have more than doubled to $2 billion. Earlier this year, AstraZeneca officials bragged to investment analysts that they expected more than 30 percent growth in sales in 2005. Recently, the company began an advertising campaign with banner ads on MySpace.com, the popular social networking Web site.
Right now, it is only FDA-approved for short-term treatment of acute mania. It is not approved for maintenance treatment of bipolar disorder, rapid cycling (switching between mania and depression), or bipolar depression. Doctors are free to prescribe it for those uses, off-label. Seroquel is now the most prescibed atypical in the U.S., according to AstraZeneca.
Almost every bipolar I’ve spoken with has had Seroquel prescribed to them because they’ve gone to their doctors complaining of insomnia—the kind of insomnia that sleeping pills cannot address. Seroquel knocks down this problem with sledgehammer efficiency. Patients tell me that they’ve generally been started at 200 milligrams and then slept well for a few weeks. Then they cannot sleep again and up goes the dosage. One patient I know wound up taking 800 milligrams a day—the amount an acute schizophrenic takes—and still couldn’t sleep. That dose of Seroquel runs $668 a month, according to drugstore.com.
All of them put on 20 to 30 pounds in short order. Most of these patients had already tried one of the other atypicals, if not two or three, before arriving at Seroquel. Interestingly, many patients I’ve interviewed began taking Seroquel in 2003 or 2004. They stuck with it for about a year, and then switched to something else in 2005 after the heavy head in the morning became too great of a trade-off. For this reason, I, too, had to stop taking the drug earlier this year.
I wonder what AstraZeneca’s executives will be telling investment analysts in 2006.
But the pharma giant recently went into press release overdrive. There was an academic conference on bipolar disorder in Holland last month. One study released at the conference claimed that Seroquel was highly effective in treating bipolar depression based on an eight-week study. Bipolar depression is a subtype of the broader disorder.
In recent interviews, several prominent researchers pointed to that study as proof of Seroquel’s efficacy in treating bipolar disorder. Some researchers said that it ought to be used long term in bipolars, as a result—and as the only drug a bipolar would take.
The study states that Seroquel worked on the depression of 53 percent of the patients in the eight-week study. That means it didn’t work for 47 percent of the patients. That’s tantalizingly close to NIMH’s own assertion that psych meds work only about half the time. It also dovetails with what patients I know have experienced on atypicals as a whole—50 percent performance.
Half-performance is wholly unacceptable. It certainly doesn’t justify a paradigm shift.
The results are even less impressive in light of what Seroquel does to patients’ bodies as well as the expense of the medication. Least impressive still is that if you are a bipolar taking an atypical like Seroquel, and you need to be to work at 8 a.m. each morning, then you’ll likely need to take your pills around 9 p.m. the previous evening. Seroquel will knock you out for a good eight hours, and you’ll need to devote two hours in the morning just to waking up. That leaves you about four hours in the evening for the rest of your life.
And they call this treating bipolar disorder? The doctors think there is solid evidence that it’s a good idea to use these meds for long-term maintenance? Why do they tout complete symptom remission as a goal, when it creates an environment where patients, who are in no position of power, are literally forced to take successively more powerful meds when doctors themselves know that complete symptom remission is a fantasy? They are kidding themselves.
Much of this shift to atypicals for treating bipolar disorder has gone on under the noses of the media and advocates for the mentally ill. Perhaps the questions that need to be asked are too subtle to permit the kind of black-and-white answers that the media love and that advocates need.
Still, it’s puzzling to me that such a vast change could be going on in the treatment of a major mental illness and the very people who should be asking the hard questions are mute. Last month, actress Linda Hamilton was a guest on Larry King Live on CNN. She was discussing her “20 years of bipolar hell.” At the top of the show, King announced that the Terminator star was also there representing Eli Lilly and their well-being approach—exercise and nutrition—for “people with serious and persistent mental illness.” In other words, she was talking to me. Too bad I wasn’t asking the questions.
King is of course no exemplar of journalistic inquisitiveness. He didn’t ask her if maybe—just maybe—those side effects and all that weight gain that she was on television saying patients needed to address were, in fact, caused by products made by Eli Lilly—namely, Zyprexa and Prozac. He didn’t ask how reasonable it was to expect someone taking Zyprexa (or Seroquel or Risperdal) in high doses to get out there and exercise and eat good food, as she was saying they must, when their weight, blood lipids, blood sugar levels, and cholesterol were shot to hell by Zyprexa. I guess looking to the media and advocates for cold-blooded honesty and accountability is naive. But someone ought to be asking serious questions because atypical antipsychotics have serious problems.
The people who most need to be held to account here are not the pharma companies, however. They are acting much as you’d expect drug companies to behave—designing drugs, calling half-performance a victory for patients, and minting money.
It’s doctors and researchers who must be held accountable. By dint of their medical degrees, they are supposed to be ethical actors. I am not convinced that it is ethical to ask millions of bipolars to take medications long term that work about as well at remitting symptoms as the old standby of a mood stabilizer plus antidepressant approach. Their proposed paradigm shift is doubly questionable given the side effects and hard-core nature of atypicals. Maybe I’ve become too much of a skeptic about psych meds, if by skeptical you understand that I actually expect meds to work and expect long-term treatments that don’t dumb down active, intelligent humans.
I still take meds, however. They are a constant in my life and will be until I die. In fact, I still have a bottle of Seroquel in my medicine cabinet. It’s there for short-term use when I cannot sleep and the edge dogs me once again, as it will. I’ll take the Seroquel just like I once took Mellaril, for a day or two, here and there.
This is an awkward time for mental- health experts, researchers, and advocates. This month, a peer-reviewed academic paper was published on the Public Library of Science Web site pointing out that researchers still have not proved the serotonin-imbalance-in-the-brain hypothesis of depression. What proof there is, the authors claim, is mostly circumstantial. Two weeks ago, The Wall Street Journal ran an article covering the same points in relation to antidepressants. And a pesky reporter was calling around the country, asking questions about bipolar disorder and atypical antipsychotics that prominent researchers hadn’t even asked themselves.
These are all matters that smart people should be willing to meet head-on.
The larger uncomfortable truth about the psychopharmacological revolution is that psychiatric medications are now part of mainstream American culture, but these meds do not consistently offer the kind of long-term benefits that many in the mental-health field claim. Nor do we fully understand the long-term consequences of their use. This is as true of antidepressants as it is of atypical antipsychotics.
That’s a lousy deal for patients, regardless of their diagnosis. It’s doubly lousy because there are no new classes of psych meds on the horizon. And any talk of gene-based cures and therapies is just talk, for now.
Meanwhile, patients have to live. They have to grapple with illnesses that are poorly understood scientifically, in an environment where medications can be as much of a problem as a solution, where incomplete evidence is the guiding light of long-term care in a revolution that’s forgotten how to serve the patient first.
The hell with that.
Atypical Antipsychotics
| Drug | Manufacturer | Black-Box Warning* | Year Introduced |
|---|---|---|---|
| Abilify (www.abilify.com) | Otsuka America | Yes | 2002 |
| Clozaril** (www.clozaril.com) | Novartis | Yes | 1989 |
| Geodon (www.geodon.com) | Pfizer | Yes | 2001 |
| Risperdal (www.risperdal.com) | Janssen | Yes | 1994 |
| Seroquel (www.seroquel.com) | AstraZeneca | Yes | 1997 |
| Zyprexa (www.zyprexa.com) | Eli Lilly | Yes | 1996 |
* A special FDA-required warning alerting consumers and doctors to known side effects of a drug, or class of drugs, owing to documented deaths or injury.
**Due to cases of toxicity, Clozaril (clozapine) is rarely prescribed.