She noticed the back pain first. Driving to the grocery store, Maryanne Clayton would have to pull over to the side of the road in tears. Then 62, a retired computer technician, she went to see a doctor in the Tri-Cities, where she lived. The diagnosis was grim. She already had Stage IV lung cancer, the most advanced form there is. Her tumor had metastasized up her spine. The doctor gave Clayton two to four months to live.
That was almost four years ago.
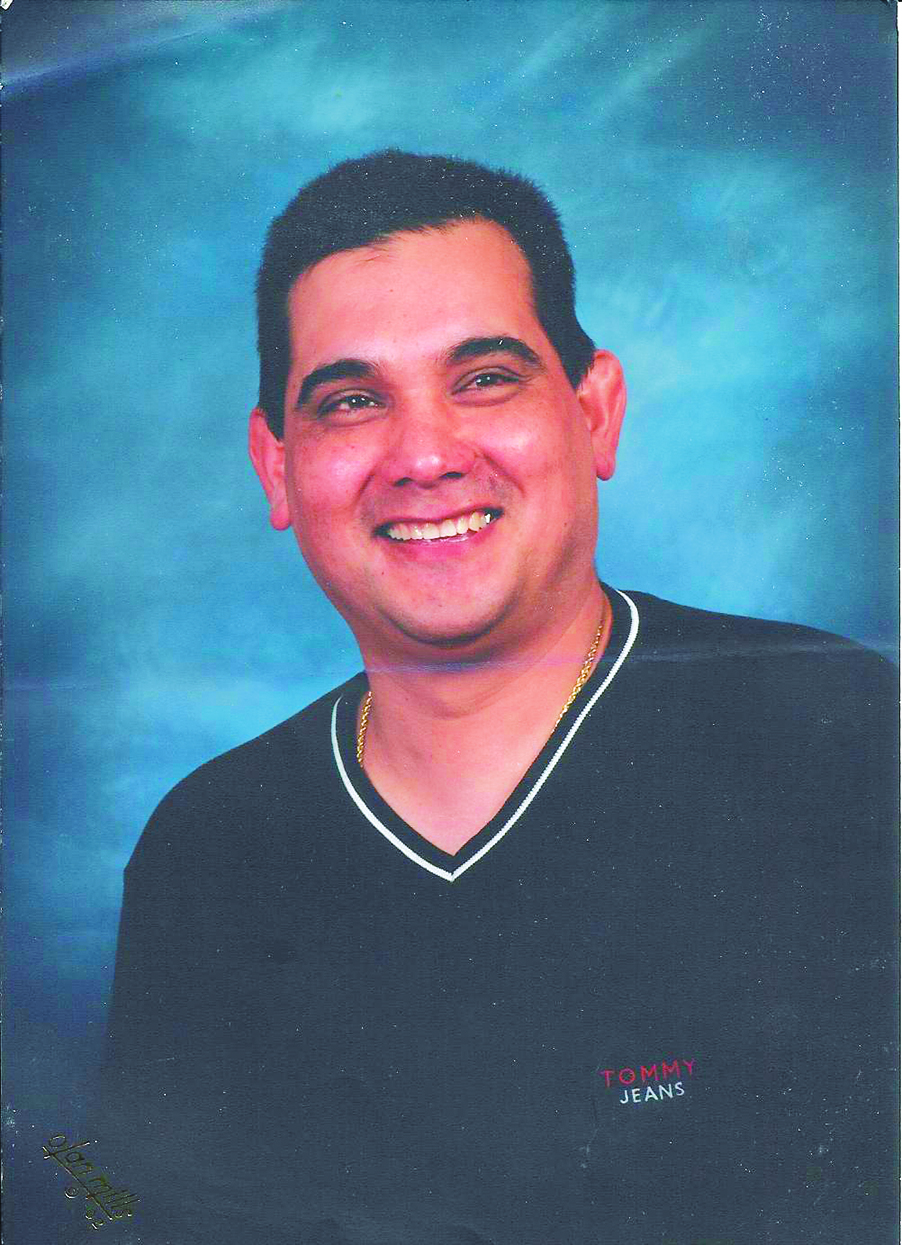
Prodded by a son who lives in Seattle, Clayton sought treatment from Dr. Renato Martins, a lung cancer specialist at Fred Hutchinson Cancer Research Center. Too weak to endure the toxicity of chemotherapy, she started with radiation, which at first made her even weaker but eventually built her strength. Given dodgy prospects with the standard treatments, Clayton then decided to participate in the clinical trial of a new drug called pemetrexate.
Her response was remarkable. The tumors shrunk, and although they eventually grew back, they shrunk again when she enrolled in a second clinical trial. (Pemetrexate has since been approved by the FDA for initial treatment in lung cancer cases.) She now comes to the Hutch every three weeks to see Martins, get CT scans, and undergo her drug regimen. The prognosis she was given has proved to be “quite wrong.”
“I just kept going and going,” says Clayton. “You kind of don’t notice how long it’s been.” She is a plain-spoken woman with a raspy voice, a pink face, and grayish-brown hair that fell out during treatment but grew back newly lustrous. “I had to have cancer to have nice hair,” she deadpans, putting a hand to her short tresses as she sits, one day last month, in a Fred Hutchinson waiting room. Since the day she was given two to four months to live, Clayton has gone with her children on a series of vacations, including a cruise to the Caribbean, a trip to Hawaii, and a tour of the Southwest that culminated in a visit to the Grand Canyon. There she rode a hot-air balloon that hit a snag as it descended and tipped over, sending everybody crawling out.
“We almost lost her because she was having too much fun, not from cancer,” Martins chuckles.
Her experience underscores the difficulty doctors have in forecasting how long patients have to live—a difficulty that is about to become even more pertinent as the Washington Death With Dignity Act takes effect March 4. The law, passed by initiative last November and modeled closely on a 14-year-old law in Oregon, makes Washington the only other state in the country to allow terminally ill patients to obtain lethal medication. As in Oregon, the law is tightly linked to a prognosis: Two doctors must say a patient has six months or less to live before such medication can be prescribed.
The law has deeply divided doctors, with some loath to help patients end their lives and others asserting it’s the most humane thing to do. But there’s one thing many on both sides can agree on. Dr. Stuart Farber, head of palliative care at the University of Washington Medical Center, puts it this way: “Our ability to predict what will happen to you in the next six months sucks.”
In one sense, six months is an arbitrary figure. “Why not four months? Why not eight months?” asks Arthur Caplan, director of the Center for Bioethics at the University of Pennsylvania, adding that medical literature does not define the term “terminally ill.” The federal Medicare program, however, has determined that it will pay for hospice care for patients with a prognosis of six months or less. “That’s why we chose six months,” explains George Eighmey, executive director of Compassion & Choices of Oregon, the group that led the advocacy for the nation’s first physician-assisted suicide law. He points out that doctors are already used to making that determination.
To do so, doctors fill out a detailed checklist derived from Medicare guidelines that are intended to ensure that patients truly are at death’s door, and that the federal government won’t be shelling out for hospice care indefinitely. The checklist covers a patient’s ability to speak, walk, and smile, in addition to technical criteria specific to a person’s medical condition, such as distant metastases in the case of cancer or a “CD4 count” of less than 25 cells in the case of AIDS.
No such detailed checklist is likely to be required for patients looking to end their lives in Washington, however. The state Department of Health, currently drafting regulations to comply with the new law, has released a preliminary version of the form that will go to doctors. Virtually identical to the one used in Oregon, it simply asks doctors to check a box indicating they have determined that “the patient has six months or less to live” without any additional questions about how that determination was made.
Even when applying the rigid criteria for hospice eligibility, doctors often get it wrong, according to Nicholas Christakis, a professor of medicine and sociology at Harvard University and a pioneer in research on this subject. As a child, his mother was diagnosed with Hodgkin’s disease. “When I was six, she was given a 10 percent chance of living beyond three weeks,” he writes in his 2000 book, Death Foretold: Prophecy and Prognosis in Medical Care. “She lived for nineteen remarkable years…I spent my boyhood always fearing that her lifelong chemotherapy would stop working, constantly wondering whether my mother would live or die, and both craving and detesting prognostic precision.”
Sadly, Christakis’ research has shown that his mother was an exception. In 2000, Christakis published a study in the British Medical Journal that followed 500 patients admitted to hospice programs in Chicago. He found that only 20 percent of the patients died approximately when their doctors had predicted. Unfortunately, most died sooner. “By and large, the physicians were overly optimistic,” says Christakis.
In the world of hospice care, this finding is disturbing because it indicates that many patients aren’t being referred early enough to take full advantage of services that might ease their final months. “That’s what has frustrated hospices for decades,” says Wayne McCormick, medical director of Providence Hospice of Seattle, explaining that hospice staff frequently don’t get enough time with patients to do their best work.
Death With Dignity advocates, however, point to this finding to allay concerns that people might be killing themselves too soon based on an erroneous six-month prognosis. “Of course, there is the occasional person who outlives his or her prognosis,” says Robb Miller, executive director of Compassion & Choices of Washington. Actually, 17 percent of patients did so in the Christakis study. This roughly coincides with data collected by the National Hospice and Palliative Care Organization, which in 2007 showed that 13 percent of hospice patients around the country outlived their six-month prognoses.
It’s not that prognostication is completely lacking in a scientific basis. There is a reason that you can pick up a textbook and find a life expectancy associated with most medical conditions: Studies have followed populations of people with these conditions. It’s a statistical average. To be precise, it’s a median, explains Martins. “That means 50 percent will do worse and 50 percent will do better.”
Doctors also shade their prognoses according to their own biases and desires. Christakis’ study found that the longer a doctor knew a patient, the more likely their prognosis was inaccurate, suggesting that doctors who get attached to their patients are reluctant to talk of their imminent demise. What’s more, Christakis says, doctors see death “as a mark of failure.”
Oncologists in particular tend to adopt a cheerleading attitude “right up to the end,” says Brian Wicks, an orthopedic surgeon and past president of the Washington State Medical Association. Rather than talk about death, he says, their attitude is “Hey, one more round of chemo!”
But it is also true that one more round of chemo, or new drugs like the one that helped Clayton, or sometimes even just leaving patients alone, can help them in ways that are impossible to predict. J. Randall Curtis, a pulmonary disease specialist and director of an end-of-life research program at Harborview Medical Center, recalls treating an older man with severe emphysema a couple of years ago. “I didn’t think I could get him off life support,” Curtis says. The man was on a ventilator. Every day Randall tested whether the patient could breathe on his own, and every day the patient failed the test. He had previously made it clear that he did not want to be kept alive by machines, according to Curtis, and so the doctor and the man’s family made the wrenching decision to pull the plug.
But instead of dying as expected, the man slowly began to get better. Curtis doesn’t know exactly why, but guesses that for that patient, “being off the ventilator was probably better than being on it. He was more comfortable, less stressed.” Curtis says the man lived for at least a year afterwards.
Curtis also once kept a patient on life support against his better judgment because her family insisted. “I thought she would live days to weeks,” he says of the woman, who was suffering from septic shock and multiple organ failure. Instead she improved enough to eventually leave the hospital and come back for a visit some six or eight months later.
“It was humbling,” he says. “It was not amazing. That’s the kind of thing in medicine that happens frequently.”
Every morning when Heidi Mayer wakes up, at 5 a.m. as is her habit, she says “Howdy” to her husband Bud—very loudly. “If he says ‘Howdy’ back, I know he’s OK,” she explains.
“There’s always a little triumph,” Bud chimes in. “I made it for another day.”
It’s been like this for years. A decade ago, after clearing a jungle of blackberries off a lot he had bought adjacent to his secluded ranch house south of Tacoma, Bud came down with a case of pneumonia. “Well, no wonder he’s so sick,” Heidi recalls the chief of medicine saying at the hospital where he was brought. “He’s in congestive heart failure.”
Then 75, “he became old almost overnight,” Heidi says. Still, Bud was put on medications that kept him going—long enough to have a stroke five years later, kidney failure the year after that, and then the onset of severe chest pain known as angina. “It was scary,” says Heidi, who found herself struggling at 3 a.m. to find Bud’s veins so she could inject the morphine that the doctor had given Bud for the pain. Heidi is a petite blond nurse with a raucous laugh. She’s 20 years younger than her husband, whom she met at a military hospital, and shares his cigar-smoking habit. Bud was a high-flying psychiatrist in the ’80s when he became the U.S. Assistant Secretary of Defense, responsible for all Armed Forces health activities.
After his onslaught of illnesses, Bud says, his own prognosis for himself was grim. “Looking at a patient who had what I had, I would have been absolutely convinced that my chance of surviving more than a few months was very slim indeed.”
Bud’s doctor eventually agreed, referring him to hospice with a prognosis of six months. That was a year and a half ago. Bud, who receives visits from hospice staff at home, has since not gotten much worse or much better. Although he has trouble walking and freely speaks of himself as “dying,” he looks like any elderly grandfather, sitting in a living room decorated with mounted animal heads, stuffing tobacco into his pipe and chatting about his renewed love of nature and the letter he plans to write to Barack Obama with his ideas for improving medical care. Despite his ill health, he says the past few years have been a wonderful, peaceful period for him—one that physician-assisted suicide, which he opposes, would have cut short.
A year after he first began getting visits from the Franciscan Hospice, the organization sent Dr. Bruce Brazina to Mayer’s home to certify that he was still really dying. It’s something Brazina says he does two to four times a week as patients outlive their six-month prognoses. Sometimes, Brazina says, patients have improved so much he can no longer forecast their imminent death. In those cases, “we take them off service”—a polite way of saying that patients are kicked off hospice care, a standard procedure at all hospices due to Medicare rules. But Brazina found that Mayer’s heart condition was still severe enough to warrant another six-month prognosis, which the retired doctor has just about outlived again.
“It’s getting to the point where I’m a little embarrassed,” Mayer says.
What’s going on with him is a little different than what happened to Randall Curtis’ patients or to Maryanne Clayton. Rather than reviving from near death or surviving a disease that normally kills quickly, Mayer is suffering from chronic diseases that typically follow an unpredictable course. “People can be very sick but go along fine and stable,” Brazina explains. “But then they’ll have an acute attack.” The problem for prognosis is that doctors have no way of knowing when those attacks will be or whether patients will be able to survive them.
When a group of researchers looked specifically at patients with three chronic conditions—pulmonary disease, heart failure, and severe liver disease—they found that many more people outlived their prognosis than in the Christakis study. Fully 70 percent of the 900 patients eligible for hospice care lived longer than six months, according to a 1999 paper published in the Journal of the American Medical Association.
Given these two studies, it’s no surprise that in Oregon some people who got a prescription for lethal medication on the basis of a six-month prognosis have lived longer. Of the 341 people who put themselves to death as of 2007 (the latest statistics available), 17 did so between six months and two years after getting their prescription, according to state epidemiologist Katrina Hedberg. Of course, there’s no telling how long any of the 341 would have lived had they not killed themselves. The Department of Health does not record how long people have lived after getting prescriptions they do not use, so there’s no telling, either, whether those 200 people outlived their prognosis. Compassion & Choices of Oregon, which independently keeps data on the people whom it helps navigate the law, says some have lived as long as eight years after first inquiring about the process (although it doesn’t track whether they ever received the medication and a six-month prognosis).
The medical field’s spotty track record with prognosis is one reason Harborview’s Curtis says he is not comfortable participating in physician-assisted suicide. It’s one thing to make a six-month prognosis that will allow patients access to hospice services, he says, and quite another to do so for the purpose of enabling patients to kill themselves. “The consequences of being wrong are pretty different,” he says.
Under the law, doctors and institutions are free to opt out, and several Catholic institutions like Providence Hospice of Seattle have already said they will do so. Medical director McCormick finds the idea of patients killing themselves particularly troubling because “you can’t predict what’s going to happen or who’s going to show up near the end of your life.” He says he has watched people make peace with loved ones or form wonderful new connections. He’s preparing a speech in case patients ask about the new law: “I will stop at nothing to ensure that you’re comfortable. I won’t shorten your life, but I will make it as high-quality as possible.”
Thomas Preston, a retired cardiologist who serves as medical director of Compassion & Choices of Washington, says he has in mind a different kind of speech: “You have to understand that this prognosis could be wrong. You may have more than six months to live. You may be cutting off some useful life.”
He also says he will advise doctors to be more conservative than the law allows. “If you think it’s going to be six months, hold off on it [writing a prescription]—just to be sure.” Instead, he’ll suggest that doctors wait until they think a patient has only one or two months to live.
The UW’s Farber leans toward a different approach. While he says he hasn’t yet decided whether he himself will write fatal prescriptions, he plans at least to refer patients to others who will. Given that prognostic precision is impossible, he says, “I personally just let go of the six months.” Instead, he says he would try to meet what he sees as the “spirit of the law” by assessing that someone is “near” the end of their life, so that he could say to them, “You’re really sick and you’re not going to get better.”
Knowing exactly when someone is going to die, he continues, is not as important as knowing when someone “has reached the point where their life is filled with so much suffering that they don’t want to be alive.”
Randy Niedzielski reached that point in the summer of 2006, according to his wife Nancy. Diagnosed with brain cancer in 2000, the onetime Lynnwood property manager had been through several rounds of chemotherapy and had lived years longer than the norm. But the cancer cells had come back in an even more virulent form and had spread to his muscle system. “He would have these bizarre muscle contractions,” Nancy recalls. “His feet would go into a cone shape. His arms would twist in weird angles.” Or his chest would of its own volition go into what Nancy calls a “tent position,” rising up from his arms. “He’d just be screaming in pain.”
Randy would have liked to move to Oregon to take advantage of the Death With Dignity Act there, according to Nancy. But he didn’t have time to establish residency as required. That was about six weeks before his death.
Nancy, who has become an advocate for physician-assisted suicide, says that typically people are only weeks or days away from death when they want to kill themselves. Oregon’s experience with people hanging onto their medicine for so long, rather than rushing to use it as soon as they get a six-month prognosis, bears this out, she says: “A patient will know when he’s at the very end of his life. Doctors don’t need to tell you.”
Sometimes, though, patients are not so near the end of their life when they’re ready to die. University of Washington bioethics professor Helene Starks and Anthony Back, director of palliative care at the Seattle Cancer Care Alliance, are two of several researchers who in 2005 published a study that looked at 26 patients who “hastened” their death. A few were in Oregon, but most were in Washington, and they brought about their own demise mostly either by refusing to eat or drink or by obtaining medication illegally, according to Back and Starks. Three of these patients had “well over six months” of remaining life, Starks says, perhaps even years.
The paper, published in the Journal of Pain and Symptom Management, quotes from an interview with one of these patients before she took her life. Suffering from a congenital malformation of the spine, she said it had reached the point that her spine or neck could be injured even while sitting. “I’m in an invisible prison,” she continued. “Every move I make is an effort. I can’t live like this because of the constant stress, unbearable pain, and the knowledge that it will never be any better.”
Under the law, she would not be eligible for lethal medication. Her case was not considered “terminal,” according to the paper. But for patients like her, the present is still unbearable. Former governor Booth Gardner, the state’s most visible champion of physician-assisted suicide, would have preferred a law that applied to everyone who viewed their suffering this way, regardless of how long they were expected to live. He told The New York Times Magazine, for a December 2007 story, that the six-month rule was a compromise meant to help insure the passage of Initiative 1000. Gardner has Parkinson’s disease, and now can talk only haltingly by phone. In an interview he explained that he has been housebound of late due to several accidents related to his lack of balance.
Researchers who have interviewed patients, their families, and their doctors have found, however, that pain is not the central issue. Fear of future suffering looms larger, as does people’s desire to control their own end.
“It comes down to more existential issues,” says Back. For his study of Washington and Oregon patients, he interviewed one woman who had been a successful business owner. “That’s what gave her her zest for life,” Back says, and without it she was ready to die.
Maryanne Clayton says she has never reached that point. Still, she voted for the Death With Dignity Act. “Why force me to suffer?” she asks, adding that if she were today in as much pain as she was when first diagnosed with lung cancer, she might consider taking advantage of the new law. But for now, she still enjoys life. Her 35-year-old son Eric shares a duplex with her in the Tri-Cities. They like different food. But every night he cooks dinner on his side, she cooks dinner on her side, and they eat together. And one more day passes that proves her prognosis wrong.