Eric Seitz grew up on the east side of Lake Washington, near Redmond, in a middle-class family. He had a bunch of cats growing up, he says, and his older brother taught him to skate and snowboard.
When he hit his teens, his parents divorced and he took to the road, spending about a decade bouncing among couches, shelters, and the streets. “I had issues with authority,” he says. “I wanted to do a bunch of hippie-punk traveling stuff, I wanted my independence as a teenager. I was pretty defiant.”
Eventually, Seitz started doing heroin, a habit that persisted until the day he found himself in a hospital about to undergo surgery. He was suffering from a flesh-eating bacteria—a condition called necrotizing fasciitis—which had found its way into his body through intramuscular injection. It was during his three-month recovery at Harborview Hospital, staring at the white tile ceiling from his hospital bed, that Seitz first became interested in medicine. He later enrolled at Central Washington University in Ellensburg, where he earned a bachelor’s in public health before attending the University of Washington for his degree in nursing. Since then, Seitz has been working in the trenches, battling two interconnected public-health crises afflicting the homeless population in Seattle and greater King County: opioid addiction and hepatitis C infections.
You’ve likely heard about the former, in these pages (see “The Spike,” Aug. 12, 2015) or elsewhere. The steep rise in the illicit use of heroin and its variants has ravaged America’s rural poor in particular—although smack is back in the big city, too, as evidenced by the limp bodies of semiconscious junkies visible on street corners across Seattle.
Hepatitis C is less obvious and therefore less notorious, but the fact that it isn’t in-your-face only makes it more dangerous. It’s particularly prevalent among baby boomers born in the two decades following World War II—the bloodborne virus can lie dormant for years or decades, and many were infected before the full discovery of hep C in 1989. Infections are growing fastest among young people, though. When hep C does manifest, it moves slowly, exhausting its victim and draining body weight. Its symptoms—including fatigue and mild confusion—can easily be mistaken for other illnesses.
Sixty-one infectious diseases trigger formal reporting with the Center for Disease Control (CDC). Hepatitis C is one, and in 2013 it killed more Americans than the other 60 combined. “I’m very frustrated by the enormous public-health failure that hep C represents,” says Steve Graham, the recently retired founder of the Hepatitis Education Project (HEP). “Not just in the recent opioid situation, but over the past 25 years. The apathy and the ignorance of officials and public policy makers … is a scandal.”
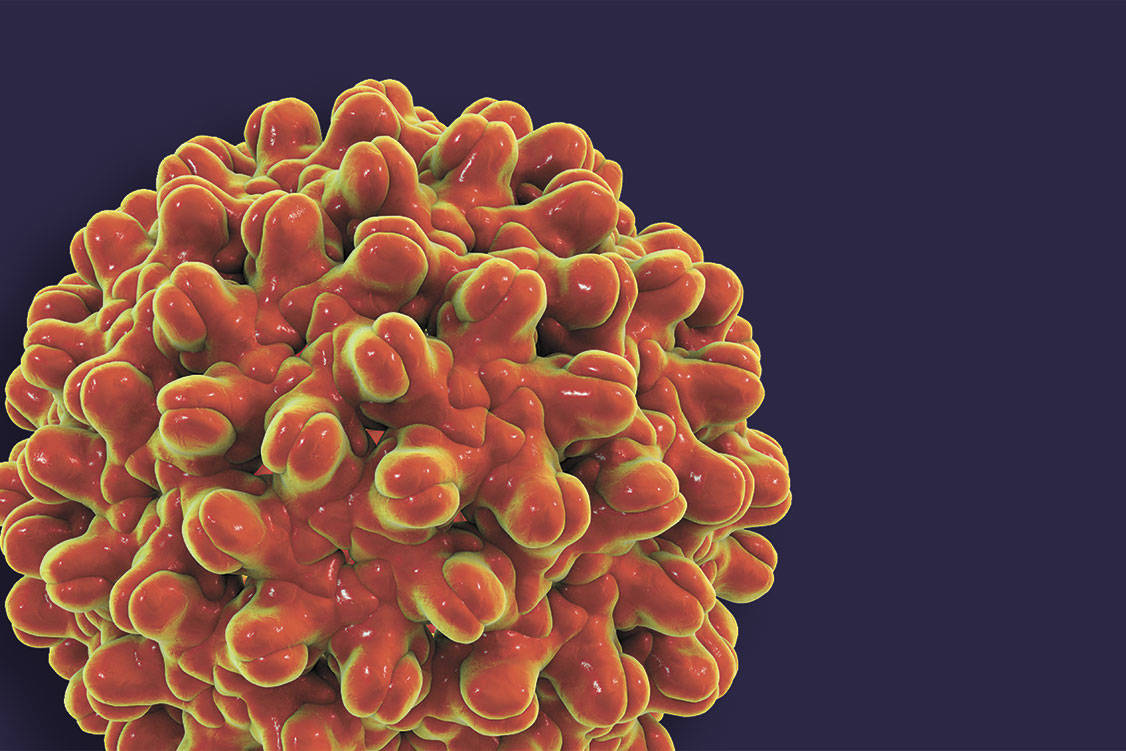
The whole ordeal begins with a single virion, smaller than a cell, sneaking into the bloodstream. At the center of the virion is RNA, the genetic instructions for creating more virions. Those instructions are encased in an inner layer of protein and an outer layer of fat, which helps the whole package burrow deep into liver cells. There the viral RNA takes control of cellular machinery to produce more virions, which are then released back into the bloodstream to infect new cells. The cell dies in the process. Much like human beings strip-mining the planet, the hep C virions gradually wear down the liver in which they live. Between 5 and 20 percent of untreated patients develop cirrhosis after two decades or so of infection; liver disease caused by hep C is the leading cause of liver transplants in the U.S. Advanced cirrhosis can cause fluid to build up inside a patient’s abdomen so that it bulges like a pregnancy.
Seitz sees the effects of hepatitis C every day in his work as a street outreach nurse. He currently works with homeless patients as they’re being evicted from unauthorized encampments—the poorest of the poor, the sickest of the sick—which presents unique challenges. He works for an agency contracted by the city (he asked us not to identify which, so that he could speak more freely). “I do a lot of wound care, mental-health referrals,” he says. “But it’s been really difficult, because usually people in that situation aren’t really worried about their medical issues. They’re worried about where they’re going to sleep the next night.” And some of them are also worried about where they will get their next fix, which is what makes them so susceptible to hepatitis C.
“Because hepatitis C is a relatively hardy virus, it can live outside the body for several days, and it can live on injection-drug-sharing equipment other than the syringe or the needle,” says Michael Ninburg, executive director of HEP. “So if a person is using a cooker or a spoon … or the cotton filter used to draw up the solution, if they’re sharing any of those and still have their own syringe and needle, they can be exposed to hepatitis C.”
While there has been a concerted effort to promote clean needle use through needle exchanges since the late 1980s in reaction to the HIV epidemic (starting illegally in Tacoma), the rest of the process of drug use has been largely neglected by authorities, meaning that hep C can spread even to users who follow HIV-based sanitation procedures when they inject. This is perhaps why the nationwide rise in heroin use over the past five years has been accompanied by a spike in hepatitis C infections. From 2011 to 2015 in Washington, the number of new cases of hepatitis C per year increased by half, and the Centers for Disease Control rates our state’s response to the disease as worse than Oregon’s, California’s, and even Idaho’s.
On paper, the spike in new infection rates has been even steeper in King County, though that’s partly because of methodological changes. While it’s hard to quantify precisely, the evidence says that the rate of new hepatitis C infections in King County is rising.
“I can’t give you an exact figure,” says Seitz, “but well over half the people I meet that are IV drug users on the street have hepatitis C.”
A collection of advocates in King County is fighting hep C by demanding access to treatment for the poorest among us. HEP is one: a nonprofit that essentially does social work for poor patients, like helping them navigate medical bureaucracy. They also recently opened a needle exchange, and are watching with bated breath as the fate of safe drug sites—the next logical step in harm reduction generally, and a way to reduce hep C transmissions specifically—is fought over in local councils, courts, and the opinion pages.
Twenty years ago, the treatment for hep C was terrible. Daily injections of a drug called interferon—made of proteins that mimic the chemical messages that an infected cell releases to warn other cells of its infection—cured about 5 percent of patients to the point that they were hep-C-free. The therapy lasted anywhere from six months to a year, and the experience overall was described by patients as “chemotherapy-lite,” says Ninburg.
Interferon gradually improved in efficacy during the ’00s, to the point of having a coin flip’s chance of working, but a true cure wasn’t available until 2013. Sofosbuvir, sold under the brand name Sovaldi, cures more than 90 percent of patients after a three- or four-month regimen of one pill a day, but it must be used in combination with other drugs that have nasty side effects. In 2014, sofosbuvir was succeeded by a miracle drug, Harvoni. It’s a combination of two other drugs, ledipasvir and sofosbuvir, both of which muck up pieces of cellular machinery used in hep C virion procreation. The regimen: one pill a day for eight to 12 weeks, with few side effects and a roughly 95 percent cure rate.
The sticker price of both medicines is about $1,000 per pill, which put the treatment out of reach for the uninsured. But even some with insurance through the Affordable Care Act didn’t have access. To save money, the state Health Care Authority (HCA), which administers Washington’s Medicaid program, Apple Health, initially barred active or recent drug users from receiving Harvoni.
Advocates objected that drug users, particularly injectors, are the group that most needs the cure, both for their own sakes and to keep them from further spreading the disease.
Ninburg recalls how in 2014 and 2015, through a lot of meetings and phone calls, HEP and other advocates gradually convinced the HCA to whittle a six-month sobriety requirement down to three months plus drug treatment. After more meetings and phone calls, they got authorities to throw out the time limit entirely in October 2015, and instead rely on “psychosocial readiness” at the discretion of the doctor. “My argument was this trumps all other issues around drug use,” says Ninburg. “If a clinician and client agree that the client is psychosocially ready, then it doesn’t matter what the drug use is.”
While the HCA budged on sobriety requirements, another obstacle for poor patients remained: a quota on scar tissue. Apple Health wouldn’t cover Harvoni for patients unless the disease had progressed enough to cause serious liver scarring. People with hep C but little scar tissue were denied. From a triage perspective, this arguably makes sense: When medicine is limited, give it to the patients who need it most.
But there was no reason for the medicine to be limited, other than cost. And from an epidemiological perspective, the quota on scar tissue was madness: Infected patients beget more infected patients. “Not identifying and treating those people just means you’re generating thousands of new cases all the time,” says Graham, “which you’re then going to have to clean up later.” As an analogy, imagine that policymakers prohibited Seattle firefighters from extinguishing house fires until the flames reach a certain height. Small fires make big fires; sick people make more people sick. That’s how infectious diseases work.
As a humanitarian side effect, the scar-tissue quota condemned patients to endure the slow ravages of hepatitis C for years, until they were sick enough to qualify for a cure. This got a lot of people’s dander up, including Amy Crewdson, an attorney with Seattle-based Columbia Legal Services. She was on the legal team that filed a lawsuit in February of last year on behalf of a pair of anonymous patients known only by the initials B.E. and A.R.
The complaint argues that in addition to slowly killing people, the HCA’s scar-tissue quota violated the rules that states agree to when they accept Medicaid money from the federal government. “Since Harvoni and other DAAs [direct-acting antivirals] meet the standard for coverage under Washington’s Medicaid program,” the complaint read, “the Medicaid Act requires coverage of the medicine when it is medically indicated” by a doctor—that is, “medically necessary.”
Superior Court Judge John C. Coughenour agreed with Crewdson that Harvoni meets that description, and in May 2016 issued a preliminary injunction that struck down Medicaid’s scar-tissue quota—in essence ordering Apple Health to pay for Harvoni for any patient who needed it. According to Cheryl Moore of the HCA, Apple Health approvals for Harvoni nearly doubled in the following year, from 1,320 to 2,372.
As a consequence, “We’re better situated here in Washington state and Seattle than probably anywhere in the country,” says Ninburg. “If you live in Washington and have hepatitis C, you will be eligible for treatment, one way or another.”
But eligibility isn’t the same as actually getting treated. And according to several service providers, it’s common for doctors to withhold Harvoni from patients who continue to use drugs or alcohol, even though state authorities don’t require it. “This is something we see around the country,” says Ninburg. “There are clinicians who see a person who is clearly an active drug user, and, rather than address the medical issues for whatever that person is in the office for, will ask or require that person to get into treatment for drug addiction, alcoholism, whatever before they’re willing to provide medical services.”
Dr. Alida Maria Gertz is a UW global health fellow with years of experience treating poor Seattleites. “As a primary care physician,” she says, “I have seen copies of notes that were written by consulting specialists on two or three occasions, in which it was written that the specialist was considering withholding treatment for a patient until that patient had stopped using drugs or alcohol.”
This is not best practice. The official guideline for hepatitis C treatment from the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America says that injection drug use “is the key driving force in the perpetuation of the epidemic … Several health models have shown that even modest increases in successful treatment of hepatitis C infection among persons who inject drugs can decrease prevalence and incidence.”
Stacy Lenny is a substance-abuse specialist in a mobile medical van run by Evergreen Treatment Services’ REACH team on contract with the city. “There’s a legacy of not treating people who are using drugs and alcohol,” she says, “as long as I’ve worked in the field. It’s only been recently, in the last couple years, that I’ve seen providers even willing to treat someone who is using drugs or alcohol.”
After Coughenour ruled against the scar-tissue quota, Crewdson began receiving calls from people who had gotten a notice that they now qualified for hep C treatment. She reckons she took maybe 200 calls over several months. “Some of those folks told me that they were actively using drugs and or alcohol, and were told by physicians that they would not get a prescription for the medication unless they got clean and sober,” she says.
Rachel Nickel, lead medical case manager for HEP, says that in her experience “a majority” of local doctors withhold medicine in order to prod patients into abstinence. It doesn’t always work, she says. Sometimes the patients are “like ‘I’m not dealing with this because I’ve been treated so poorly,’ ” says Nickels. “ ‘I’ll just die with my hep C.’ ”
“If a patient does not have someone like Rachel to help him or her,” Ninburg adds, “and is getting this pushback from their clinician … then they’re often kind of left to their own devices.”
Ninburg notes that the nature of hepatitis C makes it hard to organize patients into a constituency. During the HIV/AIDS crisis in the 1980s, gay men started dying in noticeably large numbers; the civil-rights movement that had begun at the Stonewall Inn took notice and responded with political organizing. Hep C, by contrast, takes much longer to bear symptoms, and hepatitis C patients are “generally not a community that’s easily mobilized,” says Ninburg. Many are poor and marginalized enough that they’re stuck in survival mode; others fear that coming out as a hep C patient will taint them with stigma. “Most baby boomers,” Ninburg says, “they want to get treated and cured and forget they ever had it.”
Seitz had nothing to do with the lawsuit that extended Harvoni to all hepatitis C patients on Medicaid. He was not involved in the efforts to convince the HCA to cover active drug users. But every day in the streets and underpasses of Seattle, his efforts to get the poorest, most marginalized patients back into the health-care system is aided by those prior victories.
Still, the daily churn of treating street refugees can be slow and stressful. Seitz has had more hard conversations with desperate people than he can recall, at tent encampments beneath bridges and freeways and in small, grassy fields dotted with patched tents and dented RVs. It hurts, but in a good way. “I feel it’s, I guess, a calling,” he says. “I don’t even know what that means, but I’m really comfortable with it and it means a lot to me … It’s a part of my own recovery, is trying to give back what was given to me. I have this strong sense of community with people, regardless of who they are, as human beings.
“I just like it, even though it’s really hard.”
One of Seitz’s patients, he recalls, had lived on the street for decades. The man had the stubbornness of a goat and the energy of a preteen, says Seitz. “It was rare that my priorities and his were in line, because he’d just do whatever he wanted to do. He had big issues with authority.” He had hepatitis C, and it took Seitz months of slow, gentle coaxing to finally get him to agree to a single doctor’s visit. “When he finally said, ‘Yeah, I’m ready,’ I was able to connect him immediately to a doctor at Harborview,” says Seitz. That doctor agreed to write a prescription that day and do the required labs later. “He ended up not having that bad of a cirrhosis,” says Seitz, “even though he was hep C positive for 20 years. I had to make sure that one of the case managers at his building went with him to [each follow-up] appointment a month.
“In three months, he was cured.”
cjaywork@seattleweekly.com
This article previously incorrectly stated that Seitz has a Master’s degree in nursing, and that a regimine of interferon could take as little as six weeks.