Natasha Helmick goes up for a header during a soccer match in Dallas and gets speared in the left temple by an opponent. The 14-year-old, a talented center midfielder playing in the choice Lake Highlands Girls Classic League, crumples to the ground.
She can’t see anything out of her left eye. Her coach asks if she’s OK. Natasha lies and says she’s good to go, and the coach puts her back into the lineup. She plays the remainder of the game, even though one eye sees darkness while floaters dance in front of the other.
Natasha plays again later that day, without full eyesight. Her vision eventually will return, but five years and four concussions later, she’s unable to recall much of her childhood.
Speaking to Natasha, who was forced to give up an athletic scholarship to Texas State University–San Marcos, you wouldn’t know that she is a brain-damaged 19-year-old. “But academically,” says her mother, Micky Helmick, “everything is three times harder.”
Around the time Natasha suffered her first concussion, 13-year-old Zackery Lystedt’s life changed forever. In 2006, the football player known to friends as “Ray Ray” after his idol, rampaging Baltimore Ravens linebacker Ray Lewis, was playing defense for his middle school in Maple Valley, Wash., east of Kent.
In the second quarter of a game, Zack fell backward after an unremarkable tackle and hit the back of his head. The injury escaped the notice of his father in the stands. “I thought he had gotten the wind knocked out of him,” says Zack’s father, Victor.
Zack played every down for the rest of the game, even forcing and recovering a fumble and sprinting for a 32-yard return. But when his dad met him after the game, Zack started stumbling and muttering, “My head hurts really bad.”
He collapsed onto the field. His left eye suddenly “blew out” and turned an inky black, the result of blood swelling in his skull. Then he convulsed into dozens of strokes. Says Victor, who witnessed the spectacle, helpless and confused, “My boy was dying on a football field.”
Across the country, people have awakened to the sometimes irreversible damage of concussions, especially in high-impact professional sports. With much of the attention focused on the National Football League and National Hockey League, Village Voice Media—following a months-long, nationwide investigation into the consequences of concussions on youth athletes, who are bigger and more aggressive than in past generations, and often play year-round—has found the following:
• The effect of a concussion on a kid can be much more devastating than on an adult. Doctors say that until a person is in his early to mid-20s, his or her brain is not fully developed and can’t take the same level of trauma as can an adult brain.
• Postmortem analysis, the only surefire way to measure a concussion’s devastating effects, shows that repeated blows to the head may be linked to Alzheimer’s, Parkinson’s, ALS, and a number of other fatal diseases.
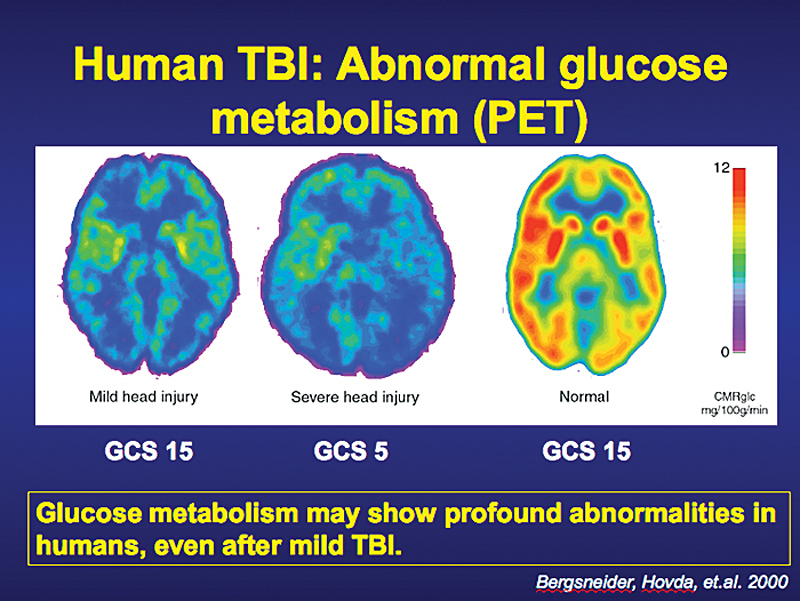
• An athlete who doesn’t exhibit outward signs of a concussion (headaches, dizziness, vomiting, temporary amnesia) can nevertheless experience changes in brain activity similar to those in a player who has been clinically diagnosed.
• Thus far in 2011, 20 state governments and the District of Columbia have signed concussion legislation that prohibits an athlete from returning to play until cleared by a licensed physician. To date, 28 states (as well as the city of Chicago) have concussion laws in place. This figure does not include Florida, whose legislators struck down a proposed bill that could have helped protect youth athletes.
• The ImPACT test, widely regarded as the go-to neurological exam to measure concussive blows, doesn’t always accurately gauge a player’s readiness to return to action. And you can cheat on it too.
Meanwhile, as attorneys debate how the new concussion laws will play out, kids like Natasha Helmick, whose memory struggles sometimes resemble those of a person three times her age, and Zackery Lystedt, who is only now beginning to walk under his own power five years later, continue to battle a condition that puts parents who want the best for their kids in a difficult spot: push them to be standouts in sports—which are often the key to a better future—or hold back on account of all the harm that can be done?
For Ali Champness, it was a freak ball, kicked into her face by her own goalkeeper in practice, that turned her life upside down. The 14-year-old freshman, who’d already made junior varsity at Garces Memorial, a Catholic high school in Bakersfield, Calif., told her parents the sting went away after a little while.
Two days later, though, on the way to a game, Ali complained of a headache and dizziness, according to her mother, Kim Champness.
During that game, the ball was kicked in the air and “brushed across the front of [Ali’s] face,” says Kim. “It was not a hard hit at all, but right after that, she started stuttering.” Ali saw a doctor, who discovered a number of much more serious problems.
In the past, a “bell ringer” was thought of the same way as a cut or a sprained ankle, with no lasting side effects. Until a few years ago, the NFL’s medical committee on concussions published studies that concluded players were not suffering long-term damage from head trauma incurred by hard hits.
The lack of awareness carried into the training rooms of every sport, says Chris Nowinski of the Boston-based Sports Legacy Institute. “Ninety percent of concussions went undiagnosed,” he says. “In fact, today you can talk to an athlete and ask the amount of concussions they’ve had and give them the actual definition, and that number will increase.”
Nowinski, a former World Wrestling Entertainment pro and author of Head Games: Football’s Concussion Crisis, along with noted neurosurgeon Dr. Robert Cantu, founded the Sports Legacy Institute. The foundation works with Boston University’s Center for the Study of Traumatic Encephalopathy in performing post-death pathology on brains donated by former athletes.
One of the latest specimens examined was that of Dave Duerson, a former NFL All-Pro safety who, following years of dementia and depression, shot himself to death—in the chest so his brain would be preserved—on February 17. Neurologists later confirmed that Duerson, who had played for the Chicago Bears, New York Giants, and Phoenix (now Arizona) Cardinals, was afflicted with chronic traumatic encephalopathy (CTE), a neurodegenerative disease linked to the total amount of distress a brain receives during a lifetime. Because a concussed person may not always exhibit classic symptoms such as headaches and nausea, CTE is, in essence, an invisible killer that can cause the brain of a 35-year-old to resemble that of an 80-year-old.
Findings like these have helped turn those running the NFL from concussion skeptics into believers, spreading the word that head trauma in sports can have deadly consequences. That belief has even trickled down to the NFL-licensed Madden video games, in which a concussed player in the yet-to-be-released Madden NFL ’12 cannot return to play after suffering the injury. In February, the league also urged all states to pass concussion legislation regarding youth athletics.
For the 75 former NFL players (including nine ex-Seahawks) who sued the league in July, alleging it concealed the dangers of the injuries for decades, it’s too little, too late. Football retirees such as Mark Duper, Ottis Anderson, and ex–University of Washington star Reggie Rogers claim that the league was careless in its false assumptions. (As of press time, the NFL planned to contest the allegations.)
Meanwhile, the proper treatment of concussions, especially in youth sports, remains a developing—and murky—science.
In 2004, Jake Snakenberg, a Denver-area high-school freshman, hit his head during a football game but assured his mother he felt ready to play again. A week later, the young fullback took another blow to the head during a game.
The shot was unremarkable, but Jake staggered to his feet before falling down. He never got back up, and was declared dead the next day from second-impact syndrome, a swelling of the brain derived from a second concussion before the symptoms of the first have passed.
These types of injuries are exacerbated in youth athletes because the human brain doesn’t metabolically or neurochemically mature until a person is in his or her early-to-mid-20s, according to Dr. Mark Ashley, the co-founder, president, and CEO of the Centre for Neuro Skills, whose clinics in Bakersfield, Calif., and Irving, Texas, specialize in traumatic brain-injury rehabilitation. Ashley is currently helping Ali Champness recover from a number of serious health issues spawned by those not-too-dramatic hits from a soccer ball in January.
On Ashley’s advice, Champness sat out the rest of the soccer season. Two months later, she joined the school’s swim team. But three weeks in, Ali called her mom from a competitive meet, panicked and convinced she needed to see a doctor.
At Ashley’s center, an MRI and CAT scan revealed bleeding in Ali’s brain. A cardiologist found that the initial concussion had deregulated Ali’s autonomic nervous system. For months, whenever Ali jogged on the treadmill, her heartbeat soared high enough to trigger cardiac arrest or stroke. She still goes to rehab three hours a day.
Concussive episodes in youth aren’t limited to soccer and football players, says Dr. William Jones, a staff physician at the Ironman Sports Medicine Institute at Memorial Hermann in Houston, Texas. In recent years, Jones has witnessed a staggering increase in concussions, due partly to better detection, in high-school cheerleaders and 10-year-old gymnasts.
Because of this broadening concept of what a concussion is and exactly which athletes are susceptible, school districts en masse are adopting new procedures for dealing with blows to the head. The most popular is the ImPACT test. A simple computer program designed by a pair of Pittsburgh doctors in the early 1990s, the exam finds an athlete’s “baseline”—his or her mental aptitude and quickness of reflexes when they’re not suffering concussive symptoms—so it can be used later in a comparative test to see if a collision has caused a lag.
But the test has hit real-world snags. The first is its price: With packages costing roughly $600 per school for the first year, ImPACT is deemed too expensive for some districts. And even when they spring for the program, few schools can afford to pay a specialist to administer it. That duty tends to fall on coaches or trainers, who are often unqualified to conduct it. And as was shown in a litigious case in the ‘burbs of New York City, the results can be tragic.
In 2008, Ryne Dougherty, a 16-year-old high-school linebacker in Essex County, N.J., sat out three weeks following a concussion. After taking an ImPACT test, he was cleared to play. But during his first game back, Ryne suffered a brain hemorrhage, slipped into a coma, and died within a week.
In their lawsuit against the school district, Ryne’s family claims that his ImPACT results were ominously low. Additionally, according to the test results, the teen reported feeling “foggy,” but was still cleared to play.
“Fogginess is the lead predictor of lasting head trauma,” says Beth Baldinger, the attorney representing Ryne’s family. “[The trainer] ignored the test results in front of her. This case screams ignorance.”
Michele Chemidlin, the trainer who administered the test, ignored phone messages and an e-mail requesting comment for this story. She told Sports Illustrated that Ryne’s test was interrupted by a “disruptive” teammate, which made the results “invalid.” But Baldinger claims that the trainer retracted that story in a recent deposition.
“She testified that she never even bothered to see Ryne’s test results,” says the attorney. “It was one of the most brutal depositions I’ve ever been involved in. She left the room crying several times.”
Kenneth Podell, a Detroit neuropsychologist and one of the creators of ImPACT, declined to comment specifically on Dougherty’s case. But he says that “in ideal circumstances,” the test should be administered not by a trainer but by a medical professional.
“It’s better than nothing,” says David Hovda, professor and director of the University of California–Los Angeles’ Brain Injury Research Center, about ImPACT. “I don’t mean any disrespect, but neuropsychological tests, which require responses and performance from individuals, are always going to have problems because there’s always going to be variances.”
One of those variances is that an athlete can cheat. In April, Indianapolis Colts quarterback Peyton Manning admitted to intentionally performing poorly on baseline exams. When and if he takes post-concussion tests, figured Manning, the league’s most marketable star, the results won’t look as bad, which means he (or anyone else who employs a similar baseline-test strategy) may be able to return immediately to play. NFL Commissioner Roger Goodell later confessed that concussion-test cheating is an issue the league needs to address.
Complicating head-trauma detection is a recently released Purdue University study concluding that youth athletes who aren’t clinically diagnosed with a concussion may still experience fundamental brain changes that may be detrimental. For two seasons, three Purdue professors tracked every practice and game hit sustained by 21 Lafayette Jefferson (Indiana) High School football players. “That’s when we started to see that about half of the kids had some level of easily measurable neurophysiological change without any concussion whatsoever,” says Purdue’s Eric Nauman. “What we think is probably happening is that since these kids don’t have any symptoms, nobody ever takes them out of the game or makes them sit. They probably keep racking up more and more hits, and it tends to affect more and more of the brain.”
Nauman and his colleagues are looking for funding so they can study soccer players, wrestlers, and participants in activities that aren’t usually thought of as dangerous. “Anecdotally, the cheerleaders at Purdue had almost as many concussions as the football players,” he says.
“No bill is better than a bad bill,” says Florida state Senator Dennis Jones, a working chiropractor who in May helped to kill a concussion law.
Florida is one of the few states to balk at concussion legislation for youth athletes, a nationwide trend that began in 2009 when Washington gave a thumbs-up to the Zackery Lystedt Law. A prototype for dozens to come, such an act requires any athlete under 18 who suffers a suspected concussion to receive written consent from a medical professional before returning to play. (There is no similar federal law.)
In Texas, Natasha’s Law, named after former soccer player Natasha Helmick, was signed by Governor Rick Perry in June after the Senate passed the bill by a 31-0 margin. And, beginning on January 1, 2012, Colorado’s Jake Snakenberg Act will take the Lystedt Law one step further by requiring every coach in youth athletics to complete an online concussion-recognition course.
Florida, however, recoiled from its own version of concussion safety because Jones was miffed that the language did not include the back-cracking set among “medical professionals.” Jones didn’t help his cause by talking on the Senate floor about how standard MRIs can be used to detect concussions, which is a fallacy. Jones filed an amendment to include chiropractors and the House refused to vote on the amended bill, which died on the floor.One of those speaking in favor of the bill, and against Jones, was David Goldstein, a “little freshman” by his own estimation, who shouldn’t even have been on the soccer pitch during the January 2010 district finals for Ransom Everglades, a Miami-area prep school, when it played longtime rival Gulliver. But when an older kid was injured, David subbed in, and was playing one of the best matches of his life when he collided head-to-head with an opponent he describes as “a monster from Gulliver.”
Game tape shows David holding his head and swaying like a drunk. But there was no way he was going to take himself out of the match, and his coach didn’t either.
It was—though David didn’t understand the medical ramifications at the time—his third concussion in four years. After the game, he felt nauseated and cowed by light, stumbling to his dad’s car and collapsing.
For months, the “blaring” headache persisted. “It’s always there,” he says. “It’s so intense, it takes over your life.” Previously a devoted student, David took refuge in the school nurse’s office three hours each day, closing his eyes to the painful light. He became agitated and impatient with his friends. Every specialist his parents took him to was perplexed by his condition.
David was told by doctors to “wait it out, never play soccer again, and good luck.” It wasn’t until he visited the University of Miami—one of the nation’s top medical centers for head trauma in student athletes—that his injury wasn’t treated as some unfathomable affliction. The doctors slowly worked him back to the point where he could return to soccer wearing a rugby helmet. Now 16, he’s a starter on varsity.
David is the son of the CEO of Royal Caribbean Cruises and attends a $28,000-a-year high school. That prompts an obvious question: If his treatment by coaches and trainers was botched, something that could have been prevented by a concussion law, what chance does a regular kid—one whose parents can’t pay every specialist in town—possibly have?
David tried to do something about that. Last year, he organized a raffle at his school and wrote letters asking for cash until he had raised $35,000, which will be donated to the Miami-Dade school district. It will pay for three to four years of ImPACT tests for every public school in the county.
As more and more states enact concussion laws, medical professionals, athletic trainers, and school administrators are wondering if these laws are actually going to help prevent a condition that’s inherently difficult to detect.
“I think the law comes up a little short,” says Saint Louis University head athletic trainer Anthony Breitbach about Missouri’s Interscholastic Youth Sports Brain Injury Prevention Act, “because a lot of these symptoms are subtle and can be easily concealed by the athlete if he or she wants to play.” Additionally, Breitbach estimates that since only half of the state’s schools can afford to employ an athletic trainer (which echoes a nationwide trend), a lot of concussions will continue to go undiagnosed, even with the new law in place.
In Arizona, on the strength of Governor Jan Brewer’s signature on House Bill 1521, the Mayo Clinic is offering free, online-based concussion tests to more than 100,000 high-school athletes. In June, the Mayo Clinic issued a press release stating that the Arizona Interscholastic Association had endorsed the baseline test, which was not true and caused an AIA attorney to threaten legal action. The two have since made up, and are partnering to test all Arizona contact athletes during the 2011–12 school year, starting with football.
Steve Hogen, athletic director of Mesa Public Schools, had concerns with Arizona’s law even before it passed. According to him, if he and his cohorts hadn’t been vocal about the bill’s language (which was consequently amended), the law would have placed an impossible load on them. “We had to make sure that all Pop Warner football kids were tested. That’s impossible. We can’t do that,” Hogen says. “What if an out-of-state group had come in and they didn’t have this concussion testing? We wouldn’t have had the resources to check.”
It isn’t only those administering concussion tests who are unsure about the future. Because a legal precedent has yet to be established on the new laws, attorneys also are divided on how potential lawsuits will play out in a courtroom.
Steven Pachman is a Philadelphia-based lawyer who has advised numerous academic institutions and athletic entities about concussion litigation. Though Pachman declines to comment about specific clients, a records search shows that he defended La Salle University in a lawsuit filed by the family of former football player Preston Plevretes, who claimed that the student had received severe brain damage because the school’s nurse and a team trainer inserted him back into play too soon following a concussion. (La Salle settled out of court for $7.5 million.)
Pachman explains that he receives a call every week from advice-seeking youth and high-school sports organizations, and “what I’m hearing from the defense perspective—’We don’t have a plan’ and ‘An athletic trainer is too expensive’—frightens me,” he says.
“The youth sports might suffer the most because of their lack of resources,” says Pachman. “A town of 80 people, like the one from Hoosiers, may not even think about potential litigation until something tragic happens.”
The parents of Zackery Lystedt are among the few who have filed suit on their child’s behalf. Airlifted to a Seattle ER on life support, Zackery had the top of his head completely removed by surgeons. He wasn’t supposed to regain consciousness.
The milestones that have come since then have been both miraculous and frustratingly glacially paced. Nine months following the strokes, Zack resumed speaking. By 13 months, he moved his left arm. After 20 months, he could once again eat. Now, five years later, Zack, 18, can walk a few steps with a cane, as he did in June when he accepted his diploma from Tahoma High School. “You get a little bit back, you want a little bit more,” says Victor Lystedt of his son’s progress. “You never get satisfied, because you had it all before.”
Zack’s parents, whose lives have been completely altered by caring full-time for their son, sued the school district for allowing him to play through his injury. The district settled, with one of its lawyers shrugging off the payout as a “business decision.”
That still offends his father. “Shame on those lawyers,” says Victor. “They can all rot in hell as far as I’m concerned. There’s nothing ‘business’ about my kid.”
Before she became an old woman at age 14, Kayla Meyer had three passions. She rode horses on her family’s farm. She was a huge reader (“Supernatural monsters kind of thing,” explains the gregarious Minnesotan when asked what books she likes). And, like seemingly every other man, woman, and child in the iced-over town of New Prague, 45 miles southwest of Minneapolis, Kayla played hockey.
In early 2009, Kayla, then age 13, was skating in a club game when a collision took her legs out from under her and she fell, hitting the back of her head. She told the coach she was fine and played the rest of the game.
When she went to the nurse with a headache the next day, she was given aspirin. When her headache persisted, a doctor administered a run-of-the-mill CAT scan, which does not detect concussions. Nothing looked amiss, so she was cleared to return to the ice.
“I’ve been skating since I was 4, at the pond near my house,” explains Kayla. “It would’ve just felt weird not to play hockey.”
Ten months later at a high-school team practice, Kayla was doing a drill she calls “mountain climbers,” a sort of butt-in-the-air pushup on skates. Exhausted, her arms slipped, and her forehead smacked the ice. The rest of the team skated to the locker room, unaware that she lay crumpled in pain. It wasn’t until the next team found her in the rink that Kayla’s mom, Mandy Meyer, received a frantic call to come to the arena.
Kayla’s head hurt so badly in the next couple of weeks that her bewildered parents called a plumber to check for carbon- monoxide leaks in their house. Her coach’s solution, according to Mom: “Put a helmet on her. Let her skate through it.”
Meyer’s head was too sensitive for her even to wear a helmet. She hasn’t played hockey since. A year and a half since that second concussion, she remains hobbled by excruciating headaches and a crippling intolerance to noise.
Kayla’s ordeal illustrates a current debate in the medical community: How long should a concussed youth sit out before returning to the ice (or field, or pitch, or wherever)?
“Some people said 10 days, others said three months,” says the Ironman Sports Medicine Institute’s Jones about a medical conference that he recently attended. Meanwhile, Dr. Mark Ashley sits somewhere in the middle. “We really need to be thinking seriously about waiting at least 30 days until a person with a concussion returns to play.”
Natasha Helmick, along with licensed physicians, believes that concussed kids also need to take time away from academics in order to fully recuperate. Natasha says that while she recovered from her injuries, she refused to miss her classes at Allen High. “Part of the reason why I’m so bad now is because I had a concussion and I played the next day and I went to school the day after that,” she says.
Former hockey player Kayla, unable to take the clatter of hallways or lunchrooms at her Minneapolis-area school, now gets to her classes five minutes late and leaves late as well. She’s missed 75 school days in two years. She eats lunch alone. Once a popular girl, she has been abandoned by all but a couple of her friends, so now she mostly hangs out with her mother’s friends.
Her plan had always been to become a vet technician so that she could take over the family business, a dog kennel on their farm. But now Kayla can’t tolerate barking. She can’t ride horses because the motion makes her sick. And while reading, she now has difficulty processing individual words on a page.
“I have reading glasses now, but I always forget them,” says Kayla, “and then I can only stand reading without my glasses for a couple of minutes, before the pain gets too bad.”
The Meyers don’t have health insurance. Sending Kayla to specialists is leaching the family’s finances. Though they try to keep it from her, she’s noticed that the ATV and the horse trailer have gone missing, pawned by her parents for cash. Next will be the horses, and one day maybe the farm itself.
There’s no end in sight for Kayla’s condition. “The physical therapists used to give us targets,” says Mandy Meyer. ” ‘It will be two weeks, two weeks.’ Now they don’t give her targets, because she’s missed so many of them.”
Though Mandy declares that her daughter’s concussion was “handled horribly inappropriately,” she won’t consider a lawsuit. “There are just too many people who messed up,” she says, including herself in that assessment.
In April, Kayla testified in front of the Minnesota Senate Education Committee in favor of a concussion bill, which would educate coaches and trainers and restrict when students can return to play. The lights and noise of the Capitol in St. Paul were a gauntlet for Kayla, but the bill passed.
She doesn’t blame anybody for her condition. “My coaches are awesome,” she says. “They just weren’t informed enough.”
As parents, coaches, and athletes try to find the proper balance between athletic participation and long-term health, Natasha, who’s studying at Texas State University to be an athletic trainer, still experiences depression and focus issues.
She says she still hasn’t moved past the disappointment of that day when Texas State decided to pull her athletic scholarship. “My doctor told me that I should never play a contact sport again in my life. He said, ‘Don’t even go out and shoot with friends. That’s how endangered your head is.'”
Natasha’s brother Zachary plays club select soccer and has “moved up the soccer ladder faster than Natasha did,” says their mother, Micky. This summer, Zachary participated in the U.S. Youth Soccer Olympic Development Program. If he keeps performing well, he could be handpicked from a pool of athletes to represent the country in national and international competition.
However, the 16-year-old, like his older sister, has suffered multiple concussions. Micky, mindful of her son’s dream as well as his long-term health, says it will be a “difficult decision” to pull Zachary from soccer if he sustains another head injury.
“He’s aggressive out there. He plays a lot like [Natasha]. It’s very scary for me,” says Micky, who adds that an incident that she and her daughter witnessed at the Texas state Capitol has contributed to her fears.
After Natasha’s initial testimony in front of the House of Representatives in Austin, she and her parents sat in a rotunda with former football players Robert Jones and N.D. Kalu. Jones won three Super Bowl rings as a linebacker with the Dallas Cowboys, while Kalu played at Rice University before embarking on a 12-year career with the Philadelphia Eagles, Washington Redskins, and Houston Texans.
As the Helmicks engaged in idle chitchat with the group, they noticed that something just wasn’t right mentally with these hulking athletes who had suffered countless concussions during their playing careers.
“When we left there for the day,” says Micky, “Natasha turned to me and said, ‘Mom, I could really tell. I hope I’m not that way when I’m their age.’ ”