Private First Class Mark Siegel set out on his first patrol in Iraq with a bad feeling in the air. The Army road on which he and fellow soldiers in the Fort Lewis–based 4th Stryker Brigade were traveling had two known hot spots for Improvised Explosive Devices. Others on the team had patrolled the road many times before without incident, but they couldn’t help worrying that their luck was running out.
Their convoy of four eight-wheel-drive combat vehicles, called strykers, drove through the forestlands of the north, a topography different from the desert that covers much of Iraq. With Siegel riding in the rear of the lead stryker, making sure nobody approached from behind, they warily passed the first IED hot spot. Nothing. As they approached the second, they paused. “We moved forward about an inch and boom,” Siegel recalls. As the IED hit, he closed his eyes. “When I opened them, it was all smoky. I looked around and saw fire. I remember hearing someone scream, ‘Climb out through the air guard hatch.'” That’s the opening at the top of the stryker.
He did and took a breath, reassuring himself that he was alive. The team leader was not so lucky. Siegel had caught a glimpse of him engulfed by flames in the stryker, “burning like a candle.” Siegel says he himself suffered a concussion, smoke-inhalation burns, and other injuries. He was eventually diagnosed with post-traumatic stress disorder (PTSD) as well, he says.
Shortly after the incident, the Army transported him back to Fort Lewis, where on May 28 he became one of approximately 20,000 Iraq War veterans so far to receive a Purple Heart.
Less than a month later, Siegel was escorted off the same Army base and instructed to sign a document stipulating that he could not return. He had been kicked out—or in military parlance, “administratively separated”—due to a urinalysis that revealed the presence of cocaine. As a result, he lost a host of benefits he might have otherwise received, including military-provided health care, disability pay, and eligibility for the GI Bill.
Siegel is one of numerous combat veterans being penalized after turning to drugs and alcohol or acting out in other ways. The Army and Navy discharged 3,300 people for drug use alone in the 2007 fiscal year (which ended September 2007) . (The two military branches did not supply figures for how many of those people had served in Iraq or Afghanistan.) Fort Lewis released nearly 200 soldiers for drug use in the first 10 months of the 2008 fiscal year—almost twice the number that it did in 2003, the year the Iraq War began.
The military’s approach troubles many people inside and outside the Armed Forces. They maintain that soldiers who are having trouble coping with their wartime experiences—often because of medical conditions like PTSD and traumatic brain injury—are being disciplined rather than helped.
“Nobody’s saying [substance-abusing soldiers] should stay in,” says Bart Stichman, co-director of the Washington, D.C.–based National Veterans Legal Services Program, which recently started an initiative to aid combat veterans facing misconduct discharges. “The question is: What kind of benefits should they have?” Stichman and others assert that the military should ensure that physically and mentally damaged soldiers are set up with medical care and other assistance.
“If you’ve honorably served in the war, then we owe you the assistance you need when you come home,” adds Steve Robinson, a longtime veterans’ activist who currently works for a Colorado-based organization called ONE Freedom that provides training on post-deployment adjustment.
Colby Vokey, a retired lieutenant colonel who until recently supervised the Marine Corps’ defense attorneys (kind of like public defenders in the civilian world) along the West Coast, puts it this way: “We send the soldier to Iraq. We break him. We have an obligation, at least, to fix him.”
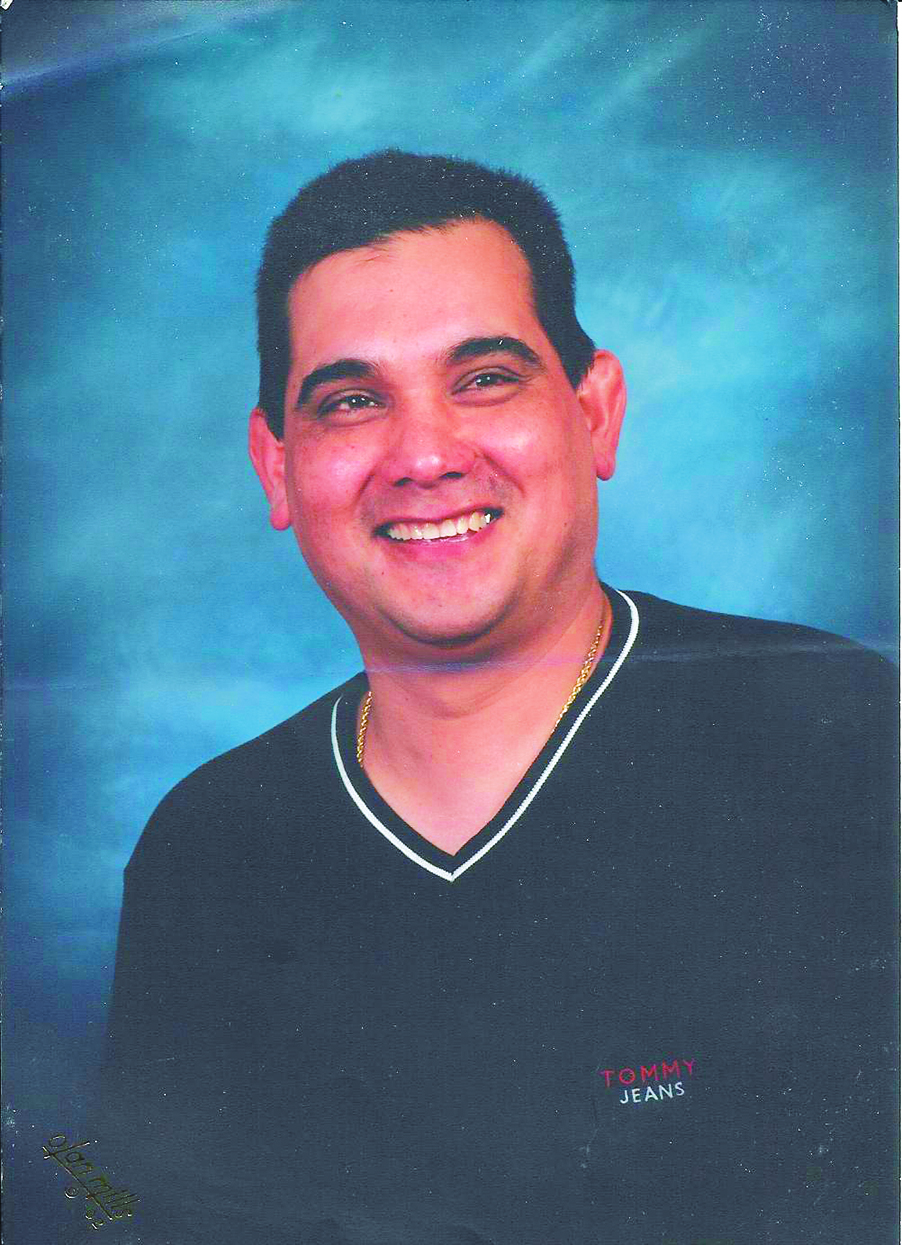
Siegel grew up in New York City. He wrote short stories and poetry and learned to play the flute, saxophone, trumpet, and guitar, among other instruments. After high school, he got a degree in computer networking and security from a vocational school. He then bounced around various tech-support jobs and had a falling-out with his parents. “I wasn’t doing anything with my life,” he says.
So at 22 he joined the Army. “It felt like I was getting my life back on track,” he says.
He made a good impression upon arriving in Iraq in October 2007. “When Mark first got there, he was a good soldier,” recalls Shenandoah Reynolds, a 30-year-old sergeant in the 4th Brigade who served alongside Siegel both in Iraq and at Fort Lewis. “He was gung-ho. He did everything right. He showed the proper respect and acted accordingly.”
A month later came the stryker explosion. Siegel says he struggled over the next couple of months as he continued his Iraq deployment. “Because I had banged up my knee, it was hard for me to keep up with my duties,” he recalls. Plus he was obsessed with the notion that he was going to die. In January the Army transported him for medical care to Landstuhl, Germany, where he was judged sick enough to send home. Back at Fort Lewis, he says he received a diagnosis of TBI and PTSD. (Fort Lewis spokesperson Joseph Piek says he cannot discuss Siegel’s medical information for privacy reasons. He did confirm the stryker incident, Siegel’s Purple Heart, and details of his military service in Iraq, which Piek described as “honorable.”)
Siegel saw a therapist on base once a week, but was still deeply troubled. “My entire body was convulsing and shaking almost daily,” he says. And he says he couldn’t sleep. Not at all.
By the time he went home to New York on a two-week leave in March, he was exhausted. Finally he fell asleep. “But every time I closed my eyes, the blast kept replaying in my head,” he says. He had visions of the enflamed stryker and the team leader he watched burn.
“I’d fall asleep and five minutes later I’d wake up. So I started drinking to see if I could black out without having any dreams. It didn’t work out that well. I wasn’t able to get drunk. So I figured, hey, if I’m not sleeping, I might as well stay awake.” That was another way of avoiding the dreams, he figured.
He turned to an old bad habit: cocaine. He says he had used the drug before joining the Army, but had been clean for a year and a half. The day he got back to Fort Lewis he had a urinalysis, which came up positive.
“I understand that I fucked up,” he said a month later by phone. “I got an Article 15 for it, that I have no problem with.” An Article 15 refers to an Army regulation that allows commanders to discipline soldiers without a court-martial. Siegel was booted down from a private first class to a private. He lost a month’s pay, and for a time his movements were restricted to his barracks and a few other places on base.
Siegel was more upset by the news that he was going to be discharged and by the constant hassling he says he was getting from his superiors. He maintains that they were trying to push him until he snapped in order to build as strong a case as possible for a discharge, a decision that rested with the brigade commander. He claims they reprimanded him for little things, like an athlete’s-foot problem he had, and required him to do onerous tasks, such as mow the lawn with a push mower. They also leaned on him, he says, when he hesitated to do things that were hard for him because of his injured knee, like moving furniture. By his own account, he was in return “abrasive and confrontational,” and quite possibly wasn’t pulling his weight.
After one scrap with a sergeant who yelled at him for disappearing to make phone calls, he says he was ordered to check in at a central desk every hour. That day in May, Siegel, who often seemed morose during several months of conversations, sounded particularly despondent. “It’s just getting really difficult,” he said.
“Mark was treated like a complete piece of crap,” affirms Reynolds. The problem, he says, is that “a lot of people thought Mark was just faking it.”
Reynolds knows firsthand how war-time trauma can cripple a man. After two tours in Iraq, a number of near-death experiences (such as stepping on a land mine that broke instead of blowing up), and the loss of many friends—including an entire squad of 14 people whom he had trained with—he finally lost it in a hotel room in Connecticut. He had gone there to visit his wife, which did not go well. He downed 28 Percocets and a quarter-bottle of rum, and got into a fight with the police who came to save him after being alerted by someone Reynolds had called to say goodbye to. He eventually was hospitalized and returned to Fort Lewis, where he also has had a hard time coping. At one time he was so spooked by the noise and the crowds on base, so convinced that somebody was out there waiting to get him, that he says he needed a few drinks in him just to walk around.
Reynolds saw the way Siegel went from being a good soldier in Iraq to one barely functioning. After the stryker explosion, Reynolds bunked next to Siegel. “He was only sleeping one or two hours a day,” Reynolds says. “He would just sit there and stare at the ceiling.”
Piek, the Fort Lewis spokesperson, won’t comment on Siegel’s discipline in detail, except to point to an Army policy that mandates the initiation of a “separation” proceeding whenever drug use is discovered. While soldiers can also be kicked out for alcohol abuse and the resulting behavior, the military takes a harsher stance on drugs, citing their illegality.
As Piek notes in a written statement, however, the start of such a procedure “does not automatically equate with actual separation.” Commanders are given leeway to decide whether or not to go through with the discharge. He declines to comment on why Siegel’s commander decided that a discharge was the right course in this case.
Army policy also requires that soldiers who test positive for drugs be referred to substance-abuse programs on the base. “Every effort is made to help a soldier rehabilitate,” says Lt. Col. George Wright, an Army spokesperson based at the Pentagon.
Yet Siegel says he was never referred to the substance-abuse program at Fort Lewis.
“It may not always happen,” admits Col. Elspeth Cameron Ritchie, a top psychiatrist for the Army’s Medical Department in Falls Church, Virginia. “One of the problems is that we don’t have enough drug and alcohol counselors. We’re trying to hire more.” The Army Substance Abuse Program at Fort Lewis, operating out of the Madigan Army Medical Center on base, employs 17 counselors, according to Madigan spokesperson Sharon Ayala. She says that number is “sufficient,” but allows that plans are in the works to hire four more.
Siegel says he didn’t particularly want counseling, since he saw his drug use as a momentary relapse. And these programs are “a double-edged sword” for soldiers anyway, notes former Marine defense attorney Vokey. Everything a soldier says about his drug and alcohol habits can be used against him in separation proceedings.
In any case, Siegel got something of a break in the end. There are three types of administrative discharges: honorable, “general under honorable conditions,” and “other than honorable.” A soldier facing a drug charge can receive the worst of the three, which may result in their being stripped of access to health care from the federal Department of Veterans Affairs (or VA). Siegel received the second type.
But while he retains VA coverage, he lost out on the possibility of military-provided health insurance, which would have allowed him to see ordinary civilian doctors, and which covers not only a soldier (for life), but also his wife and kids. This insurance is generally provided to military personnel who “medically retire.” PTSD is grounds for such a retirement. Before the drug charge, Siegel had initiated the evaluation process that determines whether a soldier’s condition warrants a medical retirement. When his urinalysis came up positive, however, that process came to a halt and his discharge proceedings began.
Siegel’s discharge also means the loss of education benefits under the GI Bill and no possibility of monthly disability payments from the military. That’s apart from losing normal retirement benefits, including a pension, that soldiers otherwise receive if they serve 20 years. Mike Colson, a retired Navy commander who coordinates outreach to War-on-Terrorism veterans for the Seattle Vet Center, says he’s seen “people 16, 18 years in [the military] losing their benefits” by getting discharged for errant behavior after coming back from Iraq or Afghanistan.
While he sympathizes with their plight, he also understands the military’s position, he says. “There are standards of behavior,” he says, “and those standards need to be enforced.”
Extensive scientific literature, dating back years, points to the relationship between PTSD, substance abuse, and other behavioral problems. Dr. Andrew Saxon, director of the addiction program at VA Puget Sound, points to one 1987 study in The New England Journal of Medicine which found that men with PTSD, including Vietnam veterans, were five times as likely to abuse drugs as others, and nearly twice as likely to be alcoholics. Describing the classic PTSD symptoms, he says those afflicted might have “unpleasant, unbidden memories, they might have nightmares, their heart might start to race, or they might react physiologically and physically to something in the environment like loud noises. You can imagine if you have those symptoms, it’s easy to reach for alcohol or obtain other drugs that temporarily help you cope.”
Captain Robert Koffman, acting director of psychological health for Navy Medicine, affirms that PTSD often brings with it other medical disorders like substance abuse. “Self-medication is typically what we see,” he says.
But the military has not fully figured out what to do with that knowledge. “It is a subject of very active debate,” says retired Captain William Nash, a psychiatrist now working as a consultant to the Marine Corps’ Defense Centers of Excellence for Psychological Health in Rosslyn, Va. “I think the issues are: Where does one draw the line in terms of responsibility and culpability? To what extent should a history of exposure to combat stress, or a diagnosis of PTSD, be considered mitigation?” Nash notes that “legally, as long as someone is not insane,” they’re considered responsible for their misdeeds. And, he says, if all combat veterans who misbehave were excused from punishment because of the trauma they’ve experienced, “it would really take away from all the other soldiers and Marines who went through those stressors and for whatever reason did not get in trouble.”
Still, Nash says, “Justice requires that whoever it is making the decision really honestly takes into account all the factors involved.” At a minimum, he says, any uncharacteristic behavior should be treated as a red flag that mental-health issues might be involved. He thus successfully urged the Marines to begin screening such individuals for PTSD and other disorders before going through with discharge proceedings. As of May, the Army has adopted a similar policy.
But the Army and Marines left unresolved the critical question of what to do after such a screening. “Whenever you have a medical diagnosis and a disciplinary action, there needs to be a decision made about which way to go forward,” says Ritchie, the Army psychiatrist. “The commander makes that final decision. In my opinion, if [the medical diagnosis] is something severe, the case should go to a medical board.” That’s the process of evaluating soldiers to see if they qualify for a medical retirement.
But Nash points out that a discharge offers one thing to commanders that the medical-retirement process does not: a “way faster” means of getting rid of a troublesome soldier. “Somebody can be out on the street in a week instead of nine months,” he says. And as Siegel’s experience shows, soldiers are continuing to be discharged even with diagnoses of PTSD in hand.
“I know there’s been a lot of progress [in recognizing that combat veterans need help],” says Reynolds, the Fort Lewis sergeant. “But down at the unit level, where the soldiers are,” it’s as though these troubled soldiers “are being swept under the rug.”
The new mental-health screening “doesn’t necessarily mean anything,” says Vokey. “It doesn’t mean the discharge proceeding stops, or they treat you any differently.” Adding to his skepticism is his past experience. Marines would come into his office with “these horrific stories,” he says. One had a best friend killed before his eyes, another’s hand couldn’t stop shaking as he talked to attorneys. About a third to a half of the Marines facing discharges had PTSD or some other mental disorder, he estimates.
Those diagnoses and experiences were “pretty much ignored,” Vokey says. He would hear arguments from commanders such as “I know PTSD is a problem, but this guy did something wrong.” And those were the leaders who believed in PTSD. “Many people, including senior leaders, did not,” Vokey says.
Petty Officer Jermie Arnold says he ran up against the nonbelieving kind. As in the Siegel case, Arnold—an Oregon native, 10-year veteran of the Navy, and recipient of a Navy/Marine Corps Achievement Medal—is currently facing a discharge from the military on a drug charge. He’s now at the Naval Station San Diego awaiting a hearing.
In early 2003, Arnold and fellow sailors were at Camp Patriot in Kuwait, where, he says, Saddam Hussein would aim missiles. At that time, nobody knew if Iraq had chemical weapons or not. And so sirens would go off warning troops to don their protective masks and suits. At 12:07 one morning, the alarm went off, and Arnold couldn’t find his mask. “I’m running everywhere looking for it,” he recalls. “Somebody had grabbed mine.” And then Arnold could see the sky light up right above him.
Still without his mask, he remembers thinking “I don’t know what I’m going to do. I’m going to sit here and die.”
He didn’t. As he leaned backwards onto somebody else’s cot and prepared for the worst, he bumped into a mask, perhaps belonging to the person who took his. He grabbed it and ran to a bunker, where he says he spent the next six hours sweating in 120-degree heat, locked in a suit that made it feel even hotter.
He was safe. But he says that since then, flashbacks of frantically looking for his mask have caused him to wake up in a cold sweat.
Upon his return in the spring of 2003, he started drinking. Each day, he says, “basically I was drinking an entire bottle of Black Velvet. It made the day go better.”
One night, after being transferred to the Naval Air Station in Kingsville, Texas, he went to a college party off base and encountered a guy shooting a cap gun. “I was freaking out,” he recalls. He left the party and went to a nearby grocery, where he grabbed some shelves leaning against a wall, intending to use them on the guy with the cap gun.
When a police officer on patrol spotted him, Arnold dropped the shelves and started running, according to both his account and Kingsville police records. The reporting officer filed charges of burglary (for stealing the shelves) and evading arrest. (They were eventually dropped for lack of evidence.)
Because of the incident, Arnold says he was called before a disciplinary review board. Arnold says he told the boardmembers that he suspected he had PTSD. It didn’t go well, he claims. “They were laughing and joking, telling me I didn’t have PTSD, saying I was just trying to get off the charges.”
The regional Navy office that covers Kingsville said they could not disclose information about Arnold’s disciplinary proceedings for privacy reasons.
His father, Tom Arnold, a former Border Patrol mechanic who lives in the Portland suburbs, wrote every member of Congress he thought could help. One, Oregon Senator Ron Wyden, launched an inquiry with the Navy, according to Tom Towslee, a spokesperson for the Senator. Towslee says the Navy reported back that Arnold had gotten medical treatment.
Not so, according to Arnold. But the Navy did transfer him for a time to a laid-back job at the Escondido Ranch, used by the Navy for bombing practice as well as for recreation for its sailors.
Still, Arnold continued to have problems as he was deployed twice more. Shortly before his third tour, he says he walked into his chief’s office and broke down crying. The chief sent him to a Navy counseling center, where he was diagnosed with PTSD, according to Arnold. But soon he was deployed again on the USS Pearl Harbor. After an R&R stop in Thailand, he tested positive for cocaine.
“I think I’ll lose all my benefits,” he now worries as he awaits his discharge hearing.
The military “should have something to help him,” bemoans his father. “They created this problem, then they just want to kick him out.”