“Frivolous suits by aggressive personal-injury lawyers are forcing medical liability premiums up and good doctors out,” proclaims literature put out by the campaign for Initiative 330, which is on the Nov. 8 ballot. It’s a high-stakes, bitterly fought measure that mirrors a sweep of proposed legislation around the country and at the federal level. Here, the initiative proposes to set a cap of $350,000 on malpractice awards for noneconomic damages, per liable health care provider or institution. I-330 also would enable injured parties to receive no more than $1,050,000 in all for such damages.
But where are these frivolous suits producing excessive, irrational payouts?
Tom Curry, executive director of the Washington State Medical Association and a spokesperson for the I-330 campaign, refers to a study published in The New England Journal of Medicine that suggests that many litigated awards are not linked to true negligence. But are there any specific Washington cases? Curry recalls a Snohomish County lawsuit that in April resulted in one of the largest malpractice jury awards in state history—$17.1 million. “I don’t know the specifics,” Curry concedes. “But I would characterize a $17 million judgment as excessive on the face of it.”
Let’s look at the specifics of the Snohomish County Superior Court case Lafferty v. Edmonds Family Medicine Clinic and Stevens Memorial Hospital. In 1998, a woman who was almost due to give birth became concerned because she couldn’t feel her baby moving. Her doctor said that she referred the woman, Tami Lafferty, to Stevens Hospital in Edmonds for a type of diagnostic ultrasound called a biophysical profile. A biophysical profile requires the ultrasound technician, or sonographer, to check for three gross body movements in a 30-minute period. There is no record of a biophysical profile being performed. Instead, there is one of what’s called a complete OB ultrasound. Dr. Arthur Castagno, Stevens’ director of radiology, describes the OB ultrasound as a better test, measuring all of the baby’s body parts. Although he wasn’t there at the time, he says he’s looked at the still pictures from the ultrasound and they “show that the fetus changed position” during the test. But he concedes that the OB ultrasound does not specifically require the sonographer to look for three body movements, and there is no evidence of such repeated movement during that examination.
What’s more, the sonographer had previously been the subject of 30 written complaints about her work, according to Lafferty’s lawyers. A disciplinary action report the month before Lafferty’s ultrasound, entered into the trial record, notes that the sonographer “performed an OB exam instead of renal.” That same month, another hospital report notes that the sonographer failed to perform the very same test, the biophysical profile, that was at issue in the Lafferty case. The hospital put the sonographer, who normally worked nights, on a week of day shifts for additional supervision, according to Lafferty’s lawyers and a trial document. But she was back working at night, unsupervised, when Lafferty came in.
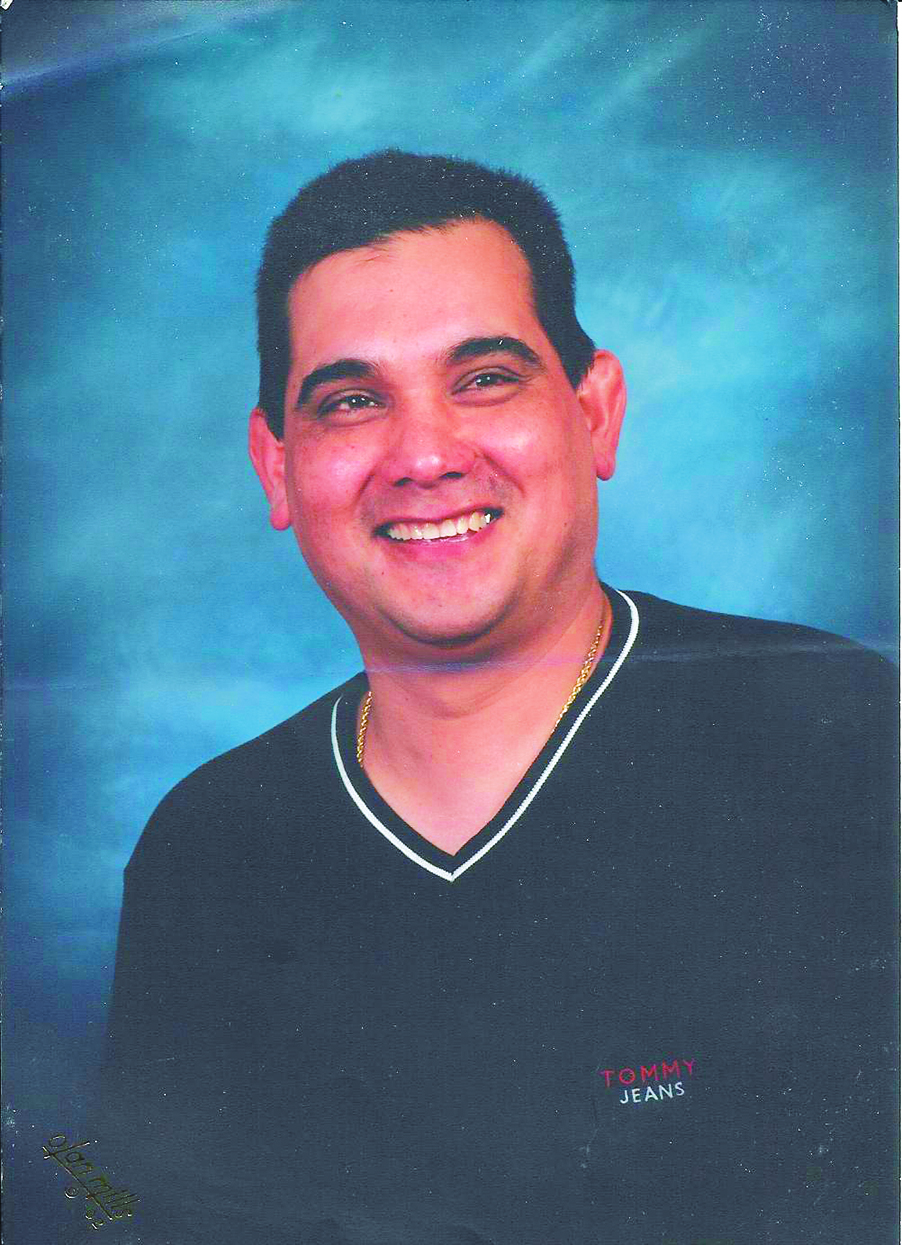
With no red flags raised from the hospital test, Lafferty didn’t see a doctor again for two days. When she did, the doctor sent her to the hospital, where her baby’s rapidly dropping heart rate became apparent. The baby was suffering from a condition that had him hemorrhaging blood inside the womb. In an emergency C-section, he was essentially stillborn. Doctors resuscitated him, but, having spent 16 minutes without oxygen, the baby suffered brain and neurological damage that has left him, now a 6-year-old named Benjamin, unable to move his limbs or talk or see properly or receive food other than from a feeding tube. His mother, all these years later, has to wake up several times a night to care for him.
Facing an appeal, Lafferty settled with the Edmonds Family Medicine clinic and its doctors after the trial for an undisclosed amount. Stevens Hospital is still appealing its 80 percent share of the jury award.
You can argue about the fine points of this case, but frivolous it is not. Even if I-330 backers could cite a recent malpractice award in Washington that, upon scrutiny, is excessive, there are several other problems with the measure’s proposal to cap awards. One is the fact that big jury awards don’t even seem to be the reason medical liability premiums have gone up.
The push for caps has a lot of resonance with doctors. With their donations, as well as those from health care institutions and insurance companies, I-330 has raised $4.8 million to date. The No on I-330 campaign has accumulated a comparatively paltry $745,000, mostly from attorneys. This big money fight might marginalize a rival medical malpractice initiative on the ballot, I-336. That’s a shame, because I-336 is an intriguing proposal to weed out bad doctors who are inexplicably allowed to engender malpractice cases time and time again.
The reason caps are so appealing is because many doctors believe that out-of-control litigation payments are responsible for sharp increases in their malpractice insurance premiums. Those premium increases are real. A few years ago, for instance, Puyallup family practice physician Edward Pullen saw his insurance premiums more than triple from $7,500 annually to $25,000. That rate took into account Pullen’s obstetrical work, one of the highest-risk areas in medicine. “It was really crazy,” Pullen says, especially since he was delivering only about 20 babies a year. And so, like many family physicians and some obstetrician-gynecologists around the state, he simply stopped delivering babies. “It’s one of the joys of family medicine I miss,” he says.
Significantly, prior to Pullen’s dramatic premium increase, he was insured through Washington Casualty, then the second- largest malpractice insurer in the state. In 2001, Washington Casualty withdrew from the malpractice market, sending a lot of clients searching for new insurance in an inhospitable market. According to state Insurance Commissioner Mike Kreidler, 2001 and 2002 were tough for the cyclical insurance market, in part due to the overall weak economy. Kreidler says conditions are changing. This year, Physicians Insurance, by far the state’s largest provider of malpractice insurance, lowered its premiums by 7.7 percent in the face of record profits.
In February, Kreidler released a study that he believes shows that malpractice litigation was not responsible for the sudden jumps in insurance premiums a few years back. The study looked at lawsuit awards, from both trials and settlements, between 1994 and 2004 paid by five malpractice insurance companies, which make up 90 percent of the state market. The study found that the payouts increased by about 9 percent a year—roughly equivalent to the rate of inflation in health care costs. “I think the most dramatic thing that data showed is that we are not seeing a spike,” Kreidler says. “It’s been fairly constant.” His research into the complex causes of insurance costs has made him turn against tort reform. A onetime optometrist and state legislator, Kreidler used to be such a big supporter that he co-sponsored legislation in 1986 that put a cap on personal injury damages. The state Supreme Court declared the cap unconstitutional, a decision that hangs over the current attempt to impose caps.
It’s not that frivolous lawsuits don’t occur, as the New England Journal of Medicine points out. And they have a visceral impact on doctors. “It’s emotionally devastating,” says Renton neurosurgeon Michael Schlitt, who has been named in nine lawsuits, several of which he describes as “junk.” He says of one that went to trial, “People are sitting there and saying these terrible things about you.” But it’s questionable whether those frivolous suits generate enough validity to produce sizable awards. It’s noteworthy that, according to Schlitt, he’s only paid money in one suit, and that was a small amount. Insurance companies still hold those suits against him, resulting in his astronomical insurance premium this year of $220,000, about double the norm for his specialty. That, however, seems more a matter to take up with the insurance company than the tort system.
There are other problems with I-330. It would limit the fees lawyers can collect in malpractice cases—on the face of it, an attractive proposition given the 30 percent to 40 percent of awards they routinely take—but only on the plaintiff side, giving the defense an unfair advantage. Most perniciously, it would enable doctors and health care organizations to require patients to sign away their right to sue them as a condition of service.
Then there is the thorny question of what’s fair compensation when negligence produces a severe injury. Curry, of the Medical Association, stresses that the caps are on noneconomic damages. They would not apply to medical expenses, or compensation for lost earnings over a person’s lifetime. Take the Lafferty case, though. Of the $17.1 million award, $5.6 million represented economic damages. Plaintiff attorney Todd Gardner points out that those economic damages don’t include care by an attendant who can relieve Lafferty from her round-the-clock duties, nor special equipment like a hydraulic lift to move her immobile son in and out of bed. Nor do those damages take into account the profound, excruciating life changes that invariably accompany an injury like her son’s. “How can you say what it’s worth if someone’s a quadriplegic?” asks fellow plaintiff’s attorney Andrew Fuller. “If he can’t talk and is blind? How do you value that?” To juror Kim Jewett, $17.1 million didn’t sound like enough. “I wanted to go higher,” she says.
The other initiative, I-336, takes a different tack on the malpractice question. “If you want to lower the cost of malpractice insurance, you have to lower the incidence of malpractice,” says Dylan Malone, a spokesperson for the 336 campaign. Malone’s now-deceased son Ian was born, like Benjamin Lafferty, with immobilizing disabilities. Ian’s delivery was marked by medical errors by several practitioners, one of whom had a string of lawsuits in his past. (See “Malpractice Assurance,” May 26, 2004.)
The most interesting of many features of I-336 would deal with repeat malpractice offenders. A three-strikes-you’re-out provision would yank the license of any doctor subject to three malpractice jury awards (but not settlements) within 10 years. Opponents argue that the provision creates an onerous climate that would pressure doctors into settling specious cases. But the bar is so high that dominant Physicians Insurance says it covers no doctors who meet that criteria, rendering its utility (and opposition to it) rather dubious.
Initiative 336 has other provisions that would change the way things are done. It would outlaw ubiquitous secrecy agreements on settlements that leave injured patients unable to talk about their cases. It would require the state to track and make public the malpractice history of every health care provider. And it would mandate a state investigation of any health care provider who made three malpractice payments (including settlements) of $50,000 or more in a five-year period.
Doctors instinctively reject I-336. “All I know is if it’s loved by lawyers, it’s by definition a bad thing,” says Stevens Hospital’s Dr. Castagno, who hasn’t yet read the initiative. In a second conversation, though, he says he’s been mulling the problem of bad doctors. “I think most doctors would be in favor of getting rid of some of these guys earlier.”
That the current system isn’t working can be seen in the case of Britt Borden, a neurosurgeon who once practiced in the same office as Schlitt. Borden paid malpractice settlements in three lawsuits, was subject to successive quality assurance actions at Valley and Overlake medical centers, and was investigated three times by the state Medical Quality Assurance Commission. And yet, throughout it all, he was permitted to keep his license, according to court and state records and attorney Stephen Bulzomi, who handled two cases against Borden. In fact, Borden moved to South Dakota, where he became entangled in another malpractice case.
In that case, Borden operated on a farmer named Marilyn Zubke who suffered a spinal fracture during an automobile accident. Zubke’s attorney, Lee Schoenbeck, claims that Borden made a mistake during surgery—which Borden denies—that increased pressure on Zubke’s spine. She had to undergo two additional operations and still feels continual pain that renders her unable to farm. But the kicker is that, according to Schoenbeck, conventional practice would dictate that Zubke didn’t need surgery at all. Borden could not be reached for comment despite calls to two of his previous lawyers and his former practice. The case was settled for an amount that is, of course, confidential.
Schoenbeck, a state legislator as well as an attorney, blames not only Borden but Washington. “Your state’s failure to regulate its medical profession appropriately has resulted in people getting maimed in my state,” he says.
Frivolous lawsuits there might be. But it’s clear the unfrivolous kind deserve as much attention in the looming battle.