Around 11:30 a.m. on July 25, 2001, Su Wilson found her 16-year-old daughter, Megan, lying in bed at their Kenmore home, her chest heaving. “Megan, get up! You have to use your medication,” Su recalls telling her daughter, who suffered from chronic asthma. According to her mother’s recollections, Megan rose from her bed and used a device called a nebulizer, which transmitted a medicinal vapor to her lungs. When that didn’t work, Su called Megan’s primary care physician, a Kirkland naturopath named Lucinda Messer.
One critical fact about that day is in dispute. Messer says that she repeatedly urged Megan and her mother to go to the hospital—and they refused. It’s noted on the medical chart from that day. But Su Wilson insists Messer never mentioned the hospital.
In any case, these things seem clear: Several hours after Megan woke up, she and her mother arrived at Messer’s office, which at the time was across the street from Evergreen Hospital. Messer was busy with another client, so an acupuncturist who worked out of the office, Dan Brown, performed acupuncture on Megan. Messer then treated Megan with a shot of vitamin B-12 and an herbal remedy called a tincture.
What Messer did not do was perform tests used by conventional medical doctors to determine the severity of an asthmatic attack and whether a patient needs to receive emergency care. There is no consensus on whether such tests should be a part of naturopathic care. But most medical doctors agree that they are essential. “The very basics were not done with this child,” says Robert Baratz, a Massachusetts internist and critic of alternative medicine who reviewed documents related to the case at the request of Seattle Weekly.
Megan and her mother went home. Some time later, with Megan still struggling to breathe, her father, Arnold Wilson, took her to Lakeshore Clinic. She lost consciousness as they drove into the parking lot and never recovered. Megan Wilson, a pretty, easygoing teenager with long, dark hair and Chinese features inherited from her mother, was pronounced dead at 6:43 p.m., the summer before her junior year of high school. She died of an attack that almost certainly would not have been fatal had she received standard hospital treatment.
The state Department of Health is investigating Messer. Unwilling to release details of an open investigation, the agency will not confirm whether the Megan Wilson case is at issue. But the timing of the investigation, launched in November, coincides with an anonymous letter the Department of Health received outlining the circumstances of Megan’s death. The case also resulted in a lawsuit by the girl’s parents against Messer and Brown.
It is a landmark case for alternative medicine in this state, both because of the tragic outcome and because it raises important questions about the standard of care to which alternative practitioners should be held.
It also reflects a new era in naturopathy, a field which, simply put, believes in using nature to heal nature. Home to the country’s most prominent school of alternative medicine, Bastyr University in Kenmore, Washington is one of only 14 states plus the District of Columbia that licenses naturopaths. In 1993, as part of a sweeping health care reform package, the state passed a law requiring insurance companies to cover services rendered by all types of licensed health care providers, including naturopaths. The move prompted several insurance plans to proffer naturopaths as primary care providers. Regence BlueShield did so. So did Boeing, which is self-insured and is where Megan’s father works the graveyard shift as a heating and refrigeration technician.
Once confined largely to providing care that supplements treatment by medical doctors, naturopaths increasingly have become the first person to which patients in all kinds of distress will turn. In April, the Legislature strengthened naturopaths’ primary care role by expanding their authority to prescribe drugs, including controlled substances such as codeine and testosterone.
The backing by the state and insurance companies has fueled naturopathy’s growth. Numbering in the dozens only a few decades ago locally, naturopaths now claim 700 license holders statewide.
“My case was the first case in Washington where natural medicine was tried—and nobody knew what they were doing,” Messer says. Actually, the case never reached trial. It was settled in 2003 for a confidential amount that Messer says was around $250,000 or $300,000. Messer’s insurance company never reported the settlement to the state Department of Health, as required by state law.
Messer herself, however, reported the case to the Naturopathic Physicians Board of Medical Examiners in Arizona, where she is also licensed. The board dismissed the case. Looking through the case file now, its executive director, Craig Runbeck, realizes that the board seemed to have considered only information supplied by Messer.
“It’s crap, bullshit stuff,” Messer says of the Wilsons’ charges of negligence. She asserts that it’s the Wilsons who are guilty of negligence for shunning conventional medical help. “There was so much neglect here,” she says. If patients ignore your advice, she asks, “What do you do? What do you do?”
Su and Arnold Wilson, who maintain that Messer never dispensed life-saving advice, see things differently. “She did not know how to handle an emergency situation,” Su Wilson says of Messer. Indeed, Su believes that neither Messer nor anybody else at her office realized that this was a life-and-death situation. “Nobody took it seriously,” Su says.
The Massachusetts internist, Robert Baratz, says doctors learn to appreciate the delicate balance between life and death. “People look OK and can be dead in five minutes. I’ve seen it happen,” Baratz says. That’s especially true with asthma. “It’s like going over a cliff. You don’t see the cliff coming until you’re over the edge.” The body finds ways to compensate for deficiencies in the lungs, masking the growing crisis until it’s too late.
That’s why tests that determine a patient’s condition are so important. Hospitals know how to deal with severe asthma attacks. They give patients intravenous steroids and other medications that cause the airways to expand. In more extreme cases, they put a tube into a patient’s airways to stimulate breathing. But first, the patient—and her health care provider—have to know that hospitalization is required. That is a central issue in Megan Wilson’s case.
“The quality of the care provided by Dr. Messer and Mr. Brown was the primary reason why Ms. Wilson died that day,” judged physician Sam Cullison, as quoted in the Wilsons’ legal brief. Cullison runs the residency program for the Providence campus in Seattle of Swedish Medical Center. “On a more probable than not basis, the patient was in status asthmaticus”— a severe state of asthmatic attack—”at the time that they originally saw her in the office and they failed to recognize that fact.
“The history taken in the note is very superficial.” Cullison was apparently referring to Messer’s chart notes from the visit. “Physical exam is wholly inadequate, and notes minimal lung exam, blood pressure and pulse. There is no note of respiratory rate.” A respiratory rate is a simple procedure, requiring only a watch, in which one counts a patient’s breaths per minute. It’s important because an asthmatic in trouble will breathe more rapidly in an attempt to get air. Messer says she believes she did a respiratory rate, though there is no record of it on the chart. Nor was there mention of an oxygenation test, done with something called a pulse oximeter, a little device that fits onto a person’s finger and measures how much oxygen is getting to the blood.
And then there was the most glaring absence on the chart. “Inexplicably, there is no peak flow noted,” Cullison was quoted in the trial brief as saying. A peak flow meter is the most basic device used to assess an asthmatic. Many have one at home. It is an inexpensive, low-tech plastic contraption with a mouthpiece into which a patient blows. The meter measures how quickly and forcefully the patient can breathe. Interviewed by phone, Cullison says that a peak flow measurement “is absolutely one of the first things I would do.”
“I don’t have a peak flow,” Messer responds. “I’m not a pulmonologist.” She maintains that most general practitioners don’t have them either. “That’s why they send patients out to specialists.”
There is some evidence that not every medical doctor uses a peak flow meter. An article this year in the Journal of Pediatric Health Care, discussing the lapses in care of asthmatic children, noted that older doctors “emphasized their own lack of training in the use of peak flow meters.” But there is broad agreement within the conventional medical world that doctors, including primary care practitioners, should be using them.
Peter McGough, chief medical officer for eight neighborhood clinics run by the University of Washington, says of the peak flow meter: “There’s no excuse for that not being in a clinic. It’s cheaper than a thermometer.”
Should the standard of care for naturopaths be any different? Not according to their critics. “There can’t be a double standard,” says Kimball C. Atwood, an anesthesiologist at Newton-Wellesley Hospital in Massachusetts who sat on a special commission on alternative medicine convened by that state. “Asthma is a very well studied disease. To do anything less than what is known to work,” he says, must be viewed as substandard care. Baratz, who heads an organization called the National Council Against Health Fraud, puts it this way: “If a person is holding himself out as a primary care provider, he damn well better do primary care.”
In investigating naturopaths, however, the state Department of Health consults only their peers, not medical doctors.
“You can’t hold a naturopathic doctor to a medical doctor standard of care, just as you can’t hold a medical doctor to a naturopathic standard of care,” asserts Daniel Labriola, a Ballard naturopath who helped write the state law regulating naturopaths and who agreed to testify on behalf of Messer. As a distinct profession, he says, naturopathy offers different but effective treatments—say, a heat wrap rather than antibiotics for a child’s earache. When naturopaths aren’t able to apply appropriate methods, they say, they will refer a patient to conventional care.
Messer and Brown’s attorney, Nancy Elliott, approached the case from that position. She pushed Cullison, during his deposition, when he stressed the importance of a peak flow reading: “Is that within the training and experience and education of a naturopath physician?”
It’s a good question. Bastyr, where Messer trained, says it does teach naturopath students to use a peak flow meter, and several Bastyr-trained naturopaths interviewed vaguely remembered that, but only one of them uses the device. “Being a primary care doctor does not mean you need to be able to treat a disease to the limits of the technology available,” Labriola says.
Some naturopaths feel, however, that the profession is evolving as it delves more deeply into primary care. In philosophy and type of treatments, naturopathy has historically operated on a different plane from conventional medicine. It stresses prevention, a holistic approach, and the “healing power of nature,” as Bastyr literature puts it. Naturopathic treatments, which might follow a very different diagnosis than offered by a medical doctor, include the use of vitamins and herbs, hydrotherapy, and homeopathy. As naturopaths venture into the mainstream, they continue to use such methods, even those like homeopathy that medical doctors feel lack a scientific basis. But they are also aware of increasing expectations that they will utilize some of the same tools as conventional health professionals, especially in health emergencies.
“I think it’s important for people to know that just because a person’s an alternative provider doesn’t mean they’re playing a different game,” says Seattle naturopath William Wulsin, who was a potential witness for the Wilsons. Mark Nolting, a naturopath as well as an acupuncturist who once chaired the acupuncture and Oriental medicine program at Bastyr, says that he would expect primary care naturopaths to have a peak flow meter and “all of that primary equipment.”
Nevertheless, Nolting agreed to serve as an expert witness for Messer and Brown. Why? “It seemed like there were additional things that could have been done,” Nolting concedes of their encounter with Megan on the day she died. “But the way I was reading the case, there was a whole prelude to coming to the office.”

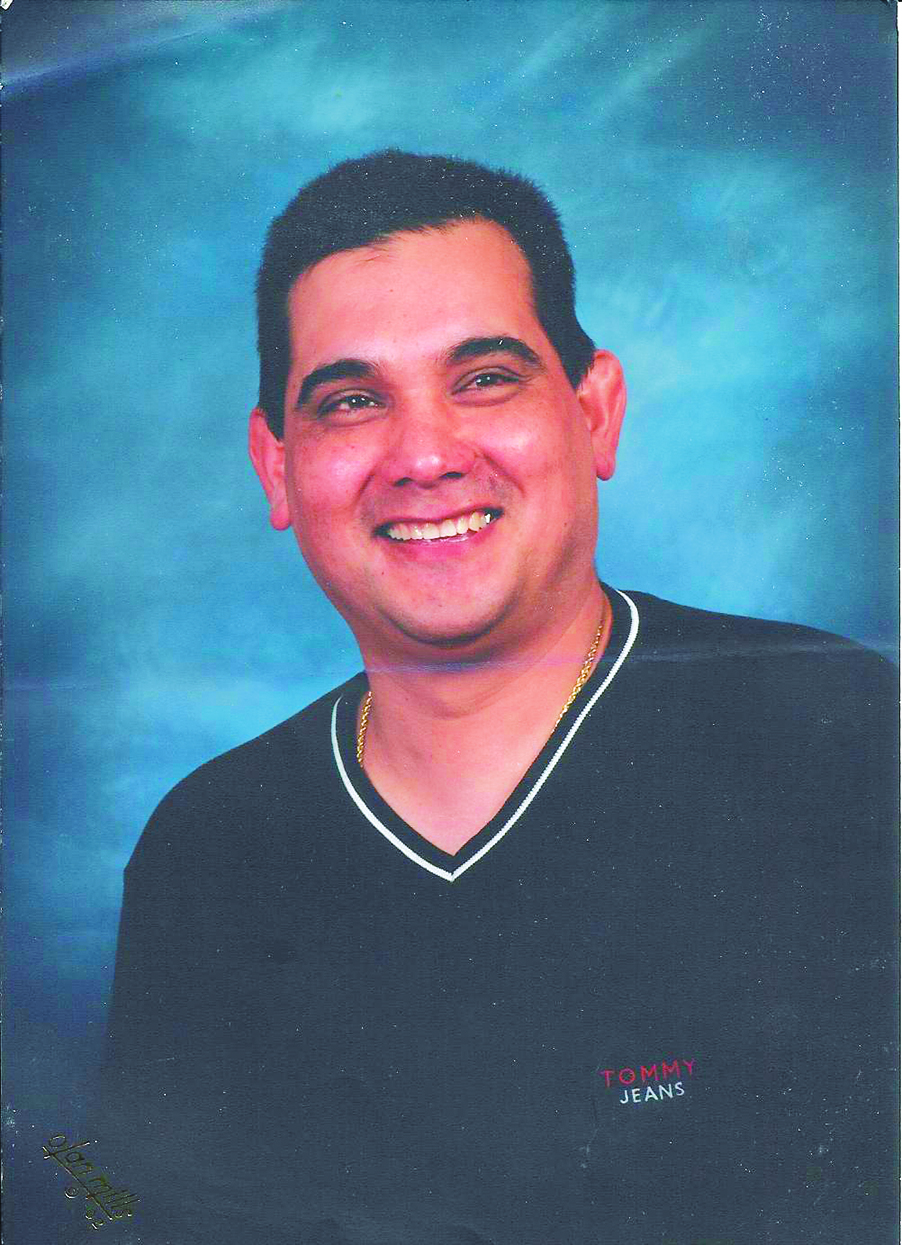
Megan Wilson, 16, died of an asthmatic attack that almost certainly would not have been fatal had she received standard hospital treatment. |
Megan Wilson and her mother first visited Messer on May 21, 1999. The middle of seven children, Megan was in many respects a typical teen. She loved animals, hanging out with friends, and dancing. She would come home from school and help her mother make dinner for the family before her father left for work. She made an impression on Messer for other reasons, though.
“Basically I remember her distinctly saying no surgeries, no accidents, never in the hospital,” the naturopath recalled during her deposition. “She was born at home by the dad, no midwife, no nurse, no doctor, never went to any doctor, never gone to any pediatrician.” Messer said she was “flabbergasted” that Arnold and Su Wilson “had seven children and no doctors in their lives.”
Providing care for several of Megan’s siblings, as well, Messer said she grew concerned about the way the parents were handling their children’s heath care. She said they refused to give antibiotics to one child who was sick. In regard to Megan, Messer said, she tried to get the teen to go to a conventional medical doctor to handle her asthma, but the girl, with support from her parents, did not wish to do so.
Messer also recalled that two years before her death, Megan had gone to a medical doctor while having an asthma attack. (They did, in fact, go to medical doctors on occasion.) The doctor wanted to keep her in the hospital overnight, but Megan declined. According to the Wilsons, Megan did so in part because Messer offered to see what she could do in lieu of hospitalization.
Messer, however, said she was so worried about the Wilsons’ parenting that she called state Child Protective Services to inquire about intervention, although she never followed up with any evidence of neglect or abuse, as the agency suggested. Messer’s legal papers contend that other health care professionals seen by Megan over the years had been similarly frustrated by the Wilsons’ noncompliance with advice. “It should have been the parents taken to court for child abuse,” says Michael Kennedy, a medical doctor at the Northwest Asthma and Allergy Center who lent his opinion to the side of Messer and Brown in the lawsuit.
According to Messer, such noncompliance continued on the day of Megan’s death. “It was a nightmarish experience,” she says of the lawsuit, which has jeopardized her ability to provide for her three children as a single mom. Not wanting to relive the experience through this article, Messer says in the middle of our conversation that if I quote her, “I’ll just say she’s full of shit and she’s lying”—”she” being me.
It’s a statement that does not help her credibility in a he-said, she-said kind of case. Nor does her contention that the Wilsons eschewed conventional medicine because Arnold was a Christian Scientist. At her deposition, when asked what the Wilsons told her about their religious background, she said, “Not much. I don’t recall specifics.” Arnold and Su Wilson, during a drive to the Bothell mausoleum where Megan rests, point out their church—the evangelical Christian Eastside Foursquare Church.
Despite her professed reluctance, Messer does talk about the case. “My husband says we are only here for herbal medicine and then we will go home,” Messer says Megan’s mother told her. Su Wilson is from Taiwan. “She’s a Chinese woman,” Messer says of Su, “very Christian, very submissive. Unfortunately, both of those breed ignorance.”
“We told her three times” to go to the hospital, Messer says. “I know my limits.” Her chart notes from that visit, a copy of which is included in the legal files, support that contention. “PT doesn’t want to go to hospital,” it reads in one place, with “doesn’t want to go” underlined.
Alternative medicine providers say they can relate to the situation. Many have had patients who believe so strongly in natural medicine and are so suspicious of the traditional medical establishment that they will have nothing to do with medical doctors—even if that goes against the recommendation of their chosen health care provider. “It’s a dilemma,” says naturopath Labriola. “It’s a really difficult place to be in. We see a lot of that in this practice. I get young women in their early 20s come in with early stage breast cancer.” He asks them if they want to do a lumpectomy; they say they want to stick with natural medicine. “I don’t throw them out the door,” he says. “The best thing you can do is to maintain a relationship with the patient.”
Labriola expressed it this way during his deposition for the Wilson lawsuit: “When patients come to a naturopathic physician with this kind of belief system, oftentimes it’s only the naturopathic physician that can lead them back to a conventional intervention that’s worthwhile.” That’s why he believes that Messer did the right thing in continuing to treat Megan even though what she evidently needed was hospitalization rather than naturopathic care. “If Dr. Messer were to have withdrawn care, chances are these patients would have gone underground, looking for other sources of information, such as the Internet, perhaps unlicensed providers,” Labriola said. The fact that she stuck with Megan, he said, “was the most positive thing” that happened in the series of events leading up to the teen’s death.
Labriola’s judgment, though, like that of other expert witnesses for Messer, assumes that her version of those events is accurate. Nothing could be further from the case, according to the Wilsons. “You don’t know how hurt I am,” says Su Wilson. “She made a huge mistake and lied about the whole thing.”
The Wilsons are sitting in their living room as they speak. They live in a rambling, dark brown house on a spacious plot of land overlooking woods. The mark of their large family is everywhere. Outside, there’s a chicken wandering around, a rabbit in a coop, and a little wooden hut, dedicated to Megan, where the family has barbecues over a pit stove. In the house are a couple of fish tanks and a comfortable clutter. Su, whose full name is Suchen, wears glasses and jeans and her dark hair in a ponytail. Her voice is full of passion. At least on this occasion, she shows no signs of submissiveness to Arnold, a native-born American who has a low-key manner and slightly disheveled hair and wears jeans and a lavender shirt. Given that Su accompanied Megan to the naturopath’s office on the day her daughter died, she initially does much of the talking.
She says when she and Megan went to the office and found the acupuncturist Dan Brown suggesting treatment while they waited for Messer, neither mother nor daughter was happy. “Megan did not want to have acupuncture,” Su says. But she says Brown told them they had to wait a half-hour for Messer in any case, and that acupuncture would help Megan breathe better. Brown, living now in Miami, declines to discuss the case. After the treatment, according to Su, Brown asked Megan if she was feeling better. “No, I feel worse,” Megan replied, says Su.
When Messer appeared, Su says, “she was very much in a hurry.” Consequently, Su claims, Messer not only failed to perform tests such as a peak flow, she never examined Megan at all. Incredible as that sounds, Su swears it is true. “She stood in the doorway and said, ‘I will come to give her a shot,'” Sue recounts. “I said, ‘Don’t you have to check Megan?'” Messer, noting that Megan was in a patient’s gown, replied, “No, go ahead, have her put her clothes back on.”
Then she treated Megan with vitamin B-12 and an herbal tincture—the tincture given, according to Su, only when she pressed the naturopath for something that would provide immediate relief. She continued to press Messer about what she should do if the treatments didn’t work, Su maintains, but the naturopath told her not to go to the ER, but to come back to the office—at noon the next day.
If, instead, Messer had urged the Wilsons to go to the hospital immediately, Su says, she would have done so. “There is no mother that would not go to the hospital when it is right across the street,” she says. “I want to tell you that.”
At the same time, the Wilsons recognize that their approach toward health care has been untraditional. “They said we didn’t follow doctors’ recommendations, which is basically true,” says Arnold Wilson. At one point, Megan was going to a medical doctor every week to monitor her asthma. Megan and her parents both found the visits useless, so they stopped going. “We weren’t getting any results from conventional medicine,” Arnold says. So they turned to naturopathy. Using such remedies as a magnesium supplement, they believed Megan had been getting stronger.
Both Arnold and Su had pasts that made them favorably inclined toward alternative medicine. “I was really sickly as a kid,” Arnold recalls. His peers used to call him “the allergy kid” because of his eczema and other ailments. He went to the doctor all the time, until he became a teenager and, like Megan, questioned whether physicians were helping. After a shouting match with one doctor, he called it quits with the conventional medical world. He started eating healthfully and reading about alternatives. Eventually, he made his way to John Bastyr, namesake of the university. The pioneering naturopath had an office on Capitol Hill. “He and I would have nice long talks,” says Arnold. “He did a hair analysis and said I was lacking a few minerals. He told me some other things to take. I started getting better.”
In time, he married Su. In her 20s, as a recent immigrant, Su had studied nursing at Shoreline Community College and for a short time worked as a nurse at Northwest Hospital in Seattle in labor and delivery. The hospital’s high cesarean section rate put her off from obstetrical medicine, so much so that when she started having her children, she chose to give birth without any medical help whatsoever.
“Over the years, we found marvelous simple treatments for a lot of things,” Arnold says. They give their kids lysine, an amino acid, for a sore throat and diluted peroxide for colds. “We don’t fear cancer around here,” Arnold says, adding that he’s in touch with groups that use natural remedies like raw foods and enzymes.
If that sounds extreme, the Wilsons maintain that they know that both alternative and conventional medicine have their place. “There are some things conventional medicine has the only good answer for,” Arnold says. An asthma attack, he says, is one of those things.
But suppose they were “natural freaks,” as Su says Messer tried to make them seem, and refused the naturopath’s urging to go to the hospital. Why, Su asks, didn’t Messer call 911 herself? It’s the same question that a range of medical doctors ask. “Essentially, I’m watching someone getting ready to die,” says McGough, the UW clinic chief, putting himself in that situation. He says he would simultaneously call the medics and take aggressive action to stabilize the patient, with nebulizer and oxygen treatments. “I’ll have that conversation”—with the parents about whether or not to hospitalize—”when the medics are there.”
“There was no reason to call an ambulance,” Messer responds. She says she wanted Megan to go to the hospital to get a rescue inhaler for possible later use. And yet, even though Messer’s chart notes say that the teen “appears to have an acute asthma attack,” Messer also contends that Megan “was not in respiratory distress. She was fine. She was laughing and talking about dinner.”
That’s not the picture Su gives, but even if it were true, how could Messer know Megan was not in respiratory distress? The naturopath had not done the necessary tests to find out.
A system based on referral to specialists is dependent on the judgment of the referring docs, whether they are naturopaths or conventional physicians. They might know their limits, but if they don’t know when a situation has surpassed those limits, they may not get a patient the help she needs. It happens in conventional medicine. Critics of naturopathy contend that the potential for such a mistake is greater in that field. The problem, according to anesthesiologist Atwood, is that naturopaths don’t “have enough experience with sick patients to know they’re really sick and when they’re not.”
Naturopaths who go through accredited programs like Bastyr’s are certainly not goofing off. Like conventional medical school, the normal program lasts four years and contains numerous courses in basic sciences: biochemistry, anatomy, neuroscience, immunology. Students learn how to perform a blood test and read an X-ray. But some of those four years are also devoted to naturopathic practices like hydrotherapy, homeopathy, and massage, so they don’t learn everything conventional medical students do.
More importantly, there is no system of required postgraduate residencies for naturopaths, as there is for medical doctors. “Every physician that I know who had trained in primary care, me included, feels strongly that medical school was only the starting point,” wrote Atwood in an article posted on the online medical service Medscape. “The residency was by far the real training ground.” A critical piece of three-year-plus residency is the time MDs spend in emergency rooms, where they see a high volume of seriously ill patients.
Kasra Pournadeali, a Marysville naturopath who heads the Washington Association of Naturopathic Physicians, points out that naturopathic students are required to have more clinical exposure than nurse practitioners, who can also practice primary care. At Bastyr, naturopathic students get 1,200 hours of clinical experience during their four-year program, most of it at the Bastyr Center for Natural Health in Seattle’s Wallingford neighborhood. Upon graduation, some naturopaths create residencies of their own.
But Bastyr spokesperson Kathleen Warren concedes that the lack of a formal residency program “is an issue. That’s our next hope.” She says Basytr would like to develop a range of postgraduate options, working with naturopaths and perhaps even MDs.
While naturopaths don’t have the training that MDs have, MDs obviously don’t have the training that naturopaths do. Naturopaths bring their own skills and treatments to the table, and in some cases that might be preferable. Warren speaks of a medical doctor who recently went through Bastyr’s naturopathy training. His “come to Jesus moment,” as she describes it, happened while operating on a 300-pound woman and realizing he was never going to be able to help her unless she did something about her obesity. That would be part of a naturopathic approach, which searches for underlying causes to illnesses.
Even some naturopaths, however, are skeptical of assorted practices in their field. “Many naturopathic interventions are poorly supported by science,” acknowledges Bellevue naturopath Bruce Klein, who wants his field to move toward an “evidence-based approach.” A former Boeing engineer who wanted a second career helping people, Klein heard about this field of natural medicine from a community college counselor and trained at Bastyr. He was wary of some of things he saw there, including alternative remedies for asthma that he felt were based more on faith than science.
In Megan Wilson’s case, the naturopathic remedies Messer used seem dubious.The Textbook of Natural Medicine, co-written by former Bastyr President Joseph Pizzorno, names vitamin B-12 as a potential asthma treatment. “I can’t even begin to think why it would be useful for asthma,” says the UW’s McGough. The textbook’s evidence? It is cited in a footnote. For one, a “personal communication” with Jonathan Wright, a controversial Seattle-area medical doctor who uses alternative methods. Secondly, the textbook cites a 1951 study in the Journal of Allergy. Looking at the now hard-to-get-hold-of study, however, reveals that although participants in a clinical trial subjectively felt an improvement in their asthma and related ailments, the objective data led the author to conclude that vitamin B-12 “is probably of no value in the treatment of chronic bronchial asthma.”
The textbook also mentions mahuang.Judging by her chart notes, that was one of several herbs used in Messer’s tincture. Mahuang is thought to help clear the airways, but it is not considered as effective as more modern drugs and contains ephedrine, which has since been banned by the federal Food and Drug Administration for its dangerous side effects.
Su and Arnold Wilson are critical of the treatments used in Megan’s case. Yet her death has not put them off natural medicine. Far from it. Most members of the family still see a naturopath as their primary care doctor: Messer’s ex-husband, in fact. Su, who says she still cries every day about losing her daughter, has learned some things, though. “After seeing Megan die, I start questioning everyone and everything,” she says. And she knows a lot more about asthma, from which other Wilson children also suffer. Her advice to them should they experience an attack: “Go to the ER.”